Background:
Cluster headache belongs to a group of primary headache disorders, classified as the trigeminal autonomic cephalalgias. Cluster headache is a neurovascular disorder characterized by recurrent, severe headaches on one side of the head, typically around the eye. There are often accompanied by autonomic symptoms during the headache such as eye watering, nasal congestion and swelling around the eye, typically confined to the side of the head with the pain.
Cluster headache is named after the demonstrated grouping of the attacks occurring collectively or together as in succession or cluster. Individuals typically experience repeated attacks of excruciatingly severe unilateral headache pain, and men are more commonly affected than women.
The exact prevalence of cluster headache in the United States is unknown, some studies estimated approximately 0.2% of the general population. It is also more prevalent in middle age men.
Pathophysiology:
The underlying etiology of cluster headache is unknown, however, about 10% of patients have a positive family history. Possible genetic factors warrant further research, current evidence for genetic inheritance is limited in data. Some research suggest that cluster headaches may be related to dysfunction of the hypothalamus, our biological clock. This theory is based on the notion that the attacks frequently occur around the same time each day.
Signs and Symptoms:
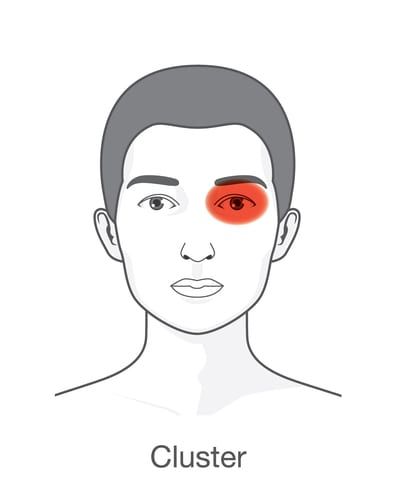
Cluster headache pain is reported as one of the most painful conditions. The pain occurs only on one side of the head (unilateral), around the eye (orbital), particularly above the eye (supraorbital), in the temple (temporal), or in any combination. The pain is typically described as severe, burning, stabbing, boring or squeezing, and may be located near or behind the orbit.
According to the diagnostic criteria developed by the International Headache Society (IHS), cluster headache has the following characteristics:
- The patient experiences attacks of severe or very severe, strictly unilateral pain (orbital, supraorbital, or temporal pain) lasting 15-180 minutes and occur from once every other day to 8 times a day
- The attacks are associated with 1 or more of the following (all on the same side): conjunctival injection, tearing, nasal congestion, rhinorrhea (runny nose), forehead and facial sweating, miosis (small pupil size), ptosis (droopy eye lid), or eyelid swelling
Cluster headache attacks often occur periodically; spontaneous remissions may interrupt active periods of pain, though about 10–15% of chronic CH never remit.
Diagnosis:
The diagnosis of a cluster headache is based on signs and symptoms. Your clinical history provides a valuable information. Neuroimaging may be necessary to rule out other medical causes of headache. The neurologist will examine you and recommend proper treatment options.
Laboratory work and radiological images should be unremarkable in cases of a cluster-type headache. Specific tests should be obtained if the history or physical examination suggests another diagnostic possibility.
A headache diary is a necessary tool for initial and correct differential diagnosis in headache conditions. It can be useful in tracking when and where pain occurs, how severe it is, and how long the pain lasts and symptoms associated with it.
Treatment Options:
Various modalities are used in the treatment of cluster headaches. Treatment involves acute (abortive) and preventive (prophylactic) therapies. Patients with frequent attacks usually require both. Acute treatments are used to stop an attack when it occurs or at least stop the progression of a headache that has started. Preventive treatments are used to reduce the frequency and severity of the attack, make acute attacks more responsive to abortive therapy, and perhaps also improve the patient’s quality of life.
The most recommended treatment of acute attacks is subcutaneous or intranasal sumatriptan. [38] Sumatriptan and zolmitriptan have both been shown to improve symptoms during an attack with sumatriptan being superior. Subcutaneous injections can be effective, in large part because of the rapidity of onset. A typical dose is 6 mg subcutaneously, which may be repeated in 24 hours or a nasal spray (20 mg) may also be helpful to abort an attack.
Dihydroergotamine can be an effective abortive agent for cluster headache. It is commonly given intravenously (IV), intranasally (0.5 mg bilaterally) or intramuscularly (IM).
Preventive therapy are also available for people with frequent and debilitating attacks to reduce the frequency and the severity of the attacks. They include different classes of medications such as calcium channel blockers and lithium. Calcium channel blockers may be the most effective agents for prophylaxis. Verapamil may be the most useful and can be combined with ergotamine or lithium.
Triggers:
Patients should avoid factors that precipitate or trigger a cluster headache. Triggers vary from person to person, some are preventable, but many are not.
Missed meals, fatigue, too much or too little sleep, anxiety can all trigger a cluster headache. Also, stress, allergens, seasonal changes, extremer temperature, alcohol or nitroglycerin may all precipitate an attack.
Resources:
National Headache Foundation
(888) NHF-5552 (643-5552)