Background:
Tension headaches are the most common type of headaches among adults, they are also known as stress headaches, with a lifetime prevalence in the general population ranging between 40% and 70% based on different studies. They often occur during the teenage years and affects women more than men.
Tension headache can be classified as episodic or chronic. An episodic tension headache may appear periodically less than 15 days per month, whereas, it is called chronic if it appears more than 15 days per month.
Pathophysiology:
There is no definite cause for tension headaches and is not an inherited trait that runs in families such as migraine headaches. In some people, tension headaches are caused by muscle spasm or tightening in the back of the neck and scalp regions. This muscle tension may be caused by stress, inadequate rest, poor posture, anxiety or fatigue.
Signs and Symptoms:
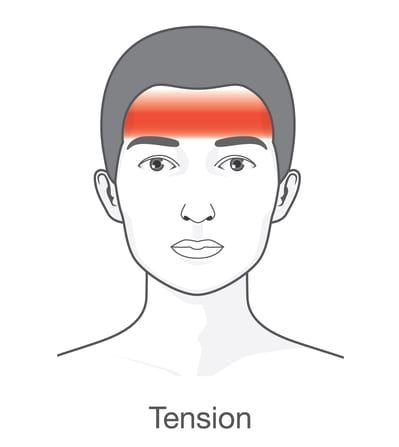
A tension headache may be described as a mild to moderate constant band-like pain, tightness, or pressure around the forehead or back of the head and neck. These headaches may last from 30 minutes to several days.
Symptoms vary greatly among people with tension headache, but the International Headache Society (IHS) diagnostic criteria states that two of the following characteristics must be present:
- Pressing or tightening (non-pulsatile quality)
- Frontal-occipital location
- bilateral – Mild/moderate intensity
- Not aggravated by physical activity
Unlike migraine headaches, there is no associated aura which often manifests as the perception of a strange light, an unpleasant smell, or blurred vision. In addition, severe sensitivity to light or noise, nausea, and vomiting are not symptoms usually associated with tension headaches.
Diagnosis:
The diagnosis of a tension headache is based on signs and symptoms. Your clinical history provides a valuable information. Neuroimaging may be necessary to rule out other medical causes of headache. The neurologist will examine you and recommend proper treatment options.
Laboratory work and radiological images should be unremarkable in cases of a tension-type headache. Specific tests should be obtained if the history or physical examination suggests another diagnostic possibility.
Treatment Options:
Various modalities are used in the treatment of tension headaches. These include hot or cold packs, ultrasound, electrical stimulation, improvement of posture, trigger point injections, occipital nerve blocks, stretching, and relaxation techniques.
Regular exercise, stretching, balanced meals, and adequate sleep may be part of a headache treatment program.
Numerous abortive medications are used to treat tension headaches. The choice for an individual patient depends on the severity of the attacks, comorbid medical condition and the patient’s treatment response. Pain-relieving drugs include nonsteroidal anti-inflammatory drugs, such as ibuprofen, naproxen, keteprofen and indomethacin. Other medication can also be used such as aspirin and acetaminophen. Over-the-counter (OTC) painkiller medications are often the first treatments recommended for tension headaches. If OTC pain relievers don’t help, your neurologist may recommend a prescription-strength pain reliever or a muscle relaxant.
Preventive therapy are also available for people with frequent and debilitating tension headaches to reduce the frequency and the severity of the attacks. They include different classes of medications such as tricyclic antidepressants, beta-blockers, calcium channel blockers, some anticonvulsants.
Cognitive and behavioral treatments can help prevent and treat tension headaches such as electromyographic (EMG) biofeedback, cognitive-behavioral therapy and possibly acupuncture.
Triggers:
Patients should avoid factors that precipitate or trigger a tension headache. Triggers vary from person to person, some are preventable, but many are not.
Missed meals, fatigue, too much or too little sleep, anxiety and stress can all affect tension headache. Patients are highly encouraged to use a daily diary to document the headaches. This is an effective and inexpensive tool to follow the course of the disease and to manage the triggers.
Resources:
National Headache Foundation
www.headaches.org
(888) NHF-5552 (643-5552)