Alzheimer’s is a neurodegenerative disease that causes the progressive deterioration of brain cells. Alzheimer’s Disease affects an estimated 5.8 million Americans, and causes more than half of all cases of dementia in the United States. Alzheimer’s disease is one of the most common diseases among older adults, with about 1 in 9 people over 65 years old having Alzheimer’s.
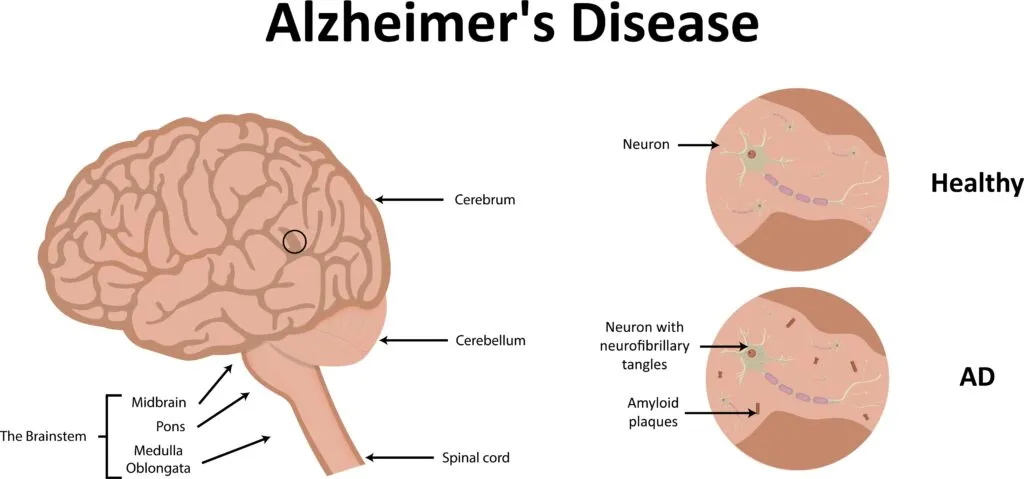
Alzheimer’s was first identified by German physician Alois Alzheimer in 1906 after he examined the brain tissue of a woman who had died from an unrelated condition and found plaques and tangles throughout her cerebral cortex and hippocampus regions of her brain. Alzheimer believed the plaques and tangles were the reason for her dementia, and Alzheimer’s is now known as a neurodegenerative disease because it causes the progressive deterioration of brain cells.
Since its initial discovery, there is still a lot that is unknown about Alzheimer’s. There are Alzheimer’s treatments available to help slow down its progression, but none have been developed to stop Alzheimer’s from worsening over time. However a recent study may bring us one step closer to understanding what causes Alzheimer’s and how to effectively treat the disease.
The Study
On September 14th, 2021, a breakthrough study on Alzheimer’s disease was published in the PLOS Biology Journal. The lead author of the study, Dr. John Mamo, Ph.D noted:
“To find new opportunities to prevent and treat Alzheimer’s, we need to understand what actually causes the disease, and presently that is not established.”
Dr. John Mamo, Ph.D
Currently, there is no known cause of Alzheimer’s. Researchers believe that it may be a combination of multiple factors such as:
- age-related changes in the brain
- genetics
- environmental factors
- lifestyle
The recent study published in PLOS Biology Journal identifies yet another possible factor that could cause Alzheimer’s disease: an abundance of toxic fat-protein complexes in the blood. It is believed that these complexes can damage capillaries and leak into the brain. Once in the brain, these complexes are believed to cause inflammation and the death of brain cells.

The Experiment
To test their hypothesis, researchers used two groups of mice. The mice in the test group were genetically modified so that their livers would produce the toxic protein of the protein-fat complex known as human amyloid-beta. The mice in the control group were not modified in any way.
Both groups of mice then had their cognitive functions evaluated using a fear-based motivated memory test. Tissue samples of the liver, brain, lung, and duodenum were also obtained from both groups of mice in order to determine the impact of amyloid-beta on these structures. This part of the experiment was performed as a blind study, meaning that researchers were not told which group the mice belonged to so they could obtain unbiased results.
The Results
The results of the study yielded some important conclusions:

- amyloid-beta proteins produced in the liver of the test mice combined with fats and traveled to the brain. Once there, these compounds disrupted the natural function of the capillaries within the brain, allowing the compounds to cross the blood-brain barrier.
- inflammation in the brain was noted in both groups of mice, however it was noted at an earlier age in the test group. The inflammation in the test group was also accompanied by degeneration in the brain cells when viewed under a microscope. While this was also present in the control group, it was rare and only affected much older mice.
- in mice of the same age, a marker of degeneration was two times greater in test mice than in control mice. As a result, the test mice were only able to perform about half as well as the control mice in retained learning tests.
What This Means:
The results of this experiment allowed researchers to learn more about how amyloid-beta affects the brain and how it can potentially lead to Alzheimer’s disease. Understanding this relationship can help to develop effective treatments that can either treat the disease and/or slow down its progression. However, it is important to note that there are limitations to this study, the most important being that testing was only performed on mice. More research is needed before introducing human subjects, but this study is a step in the right direction.

Dr. Kashouty, a diplomate of the American Board of Psychiatry and Neurology (ABPN), practices general neurology with fellowship trained specialization in clinical neurophysiology. Dr. Kashouty finds the form and function of the nerves and muscles the most interesting part of neurology, which is what led him to specialize in neurophysiology with more emphasis on neuromuscular conditions. He treats all neurological diseases, but his main focus is to treat and manage headaches, movement disorders and neuromuscular diseases.