Background:
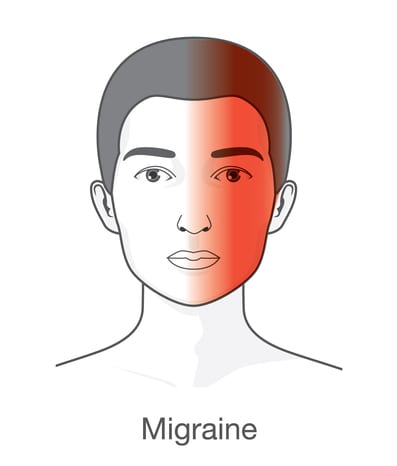
A migraine is a complex neurovascular disorder characterized by recurring moderate to severe episodes of headache. The pain typically occurs on one side of the head. It is typically a throbbing or pulsatile pain. While it is more common in women, it can affect anyone and it may begin in childhood, adolescence, or young adulthood.
Pathophysiology of Migraine:
The neurovascular theory holds that a complex series of neural and vascular events initiate migraine. According to this theory, migraine is primarily a neurogenic process with secondary changes in the cerebral perfusion. At baseline, a person has a state of neuronal hyper-excitability in the cerebral cortex, especially in the occipital cortex before the migraine attack.
The underlying causes of migraines are unknown, however, it has a strong genetic component to it as more than 65% of patients have a first degree relative with history of migraine.
Signs and Symptoms:
Few people with migraine have warning signs before the headache typically starts, a phenomenon called an aura. An aura often manifests as the perception of a strange light, an unpleasant smell, confusing thoughts or numbness on one side of the body. In few cases, people experience the aura without an accompanying headache.
Symptoms vary greatly among people with migraine, but typically headache can last up to 72 hours and has at least 2 of the following characteristics:
- Unilateral (one sided) location
- Pulsating quality
- Moderate or severe intensity (prohibits daily activities)
- Aggravation by routine physical activity
Some patients may also have sensitivity to bright light or sound, others may have nausea and/or vomiting with the headache.
Diagnosis:
The diagnosis of a migraine is based on signs and symptoms. Your clinical history provides a valuable information. Neuroimaging may be necessary to diagnose migraine to rule out other medical causes of headache. The neurologist will examine you and recommend proper treatment options.
Laboratory work and radiological images should be unremarkable in cases of a migraine-type headache. Specific tests should be obtained if the history or physical examination suggests another diagnostic possibility.
A headache diary is a necessary tool for initial and correct differential diagnosis in headache conditions. It can be useful in tracking when and where pain occurs, how severe it is, and how long the pain lasts and symptoms associated with it.
Treatment Options:
Migraine treatment involves acute (abortive) and preventive (prophylactic) therapies. Patients with frequent attacks usually require both. Acute migraine treatments are used to stop an attack when it occurs or at least stop the progression of a headache that has started. Preventive treatments are used to reduce the frequency and severity of the migraine attack, make acute attacks more responsive to abortive therapy, and perhaps also improve the patient’s quality of life.
Numerous abortive medications are used to treat migraine. The choice for an individual patient depends on the severity of the attacks, associated symptoms such as nausea and vomiting, comorbid medical condition, and the patient’s treatment response. Migraine-specific abortive treatments include prescription migraine drugs that belong to triptans such as Sumatriptan (Imitrex), Zolmitriptan (Zomig), Rizatriptan (Maxalt), Almotriptan (Axert), Eletriptan (Relpax), Naratriptan (Amerge), Frovatriptan (Frova). Although the triptans share a common mechanism of action, they differ in the available routes of administration, onset of action, and duration of action. Routes of administration include oral, intranasal, subcutaneous, and intramuscular. All the triptans are most effective when taken early during a migraine and all may be repeated in 2 hours as needed, with a maximum of 2 doses daily.
Other migraine-specific abortive treatments include ergot alkaloids such as dihydroergotamine (DHE). However, other non-migraine specific pain-relieving drugs include nonsteroidal anti-inflammatory drugs, such as ibuprofen, analgesics, such as aspirin, acetaminophen, or a drug that combines acetaminophen along with aspirin and caffeine. Patients with nausea and vomiting at the onset of an attack may respond to anti-nausea drugs.
Preventive therapy are available for people with frequent and debilitating migraines to reduce the frequency of the attacks. They include different classes of medications such as tricyclic antidepressants, beta-blockers, calcium channel blockers, some anticonvulsants. Alternative treatments, such as vitamin B2, magnesium, and CoQ-10 can be helpful in reducing the frequency of the attacks.
Cognitive and behavioral treatments can help prevent and treat migraine such as electromyographic (EMG) biofeedback, cognitive-behavioral therapy and possibly acupuncture.
Botulinum Toxin Injections:
This agent is FDA approved for the prophylaxis of chronic migraine headaches. Injections of botulinum toxin (Botox, Dysport, etc.) may be beneficial in patients with intractable migraine headaches that fail to respond to at least 3 conventional preventive medications. One of several toxins produced by Clostridium botulinum, is onabotulinumtoxin-A which blocks neuromuscular transmission in muscles. Injections of the drug, which are administered to the scalp and temple regions, may reduce the frequency and severity of migraine attacks after 2-3 months of injections.
Triggers Management:
Patients should avoid factors that precipitate or trigger a migraine attack. Triggers vary from person to person, some are preventable, but many are not.
Missed meals, alcohol, foods with monosodium glutamate (MSG), caffeine, preserved food with nitrates or nitrites, too much or too little sleep and stress can all affect migraine. Other factors that can influence your migraine include hormonal changes during the menstrual cycle, weather changes, bright or glaring lights, strong odors, and high altitude.
Patients are highly encouraged to use a daily diary to document the headaches. This is an effective and inexpensive tool to follow the course of the disease and to discover the triggers.
Resources:
American Migraine Foundation
www.americanmigrainefoundation.org
(856) 423-0043
Migraine Research Foundation
www.migraineresearchfoundation.org
(212) 249-5402
National Headache Foundation
www.headaches.org
(888) NHF-5552 (643-5552)