Everyone gets the occasional headache, and some people may have more frequent headaches than others. While the majority of headaches are not serious and will eventually resolve themselves, there are certain cases where a headache can be a symptom of something more serious, like a stroke. However, it can be hard to distinguish a benign headache from a stroke-related headache. In order to help you know the difference, here is more information about strokes, stroke-related headaches, and what a stroke-related headache feels like.
What is a stroke?
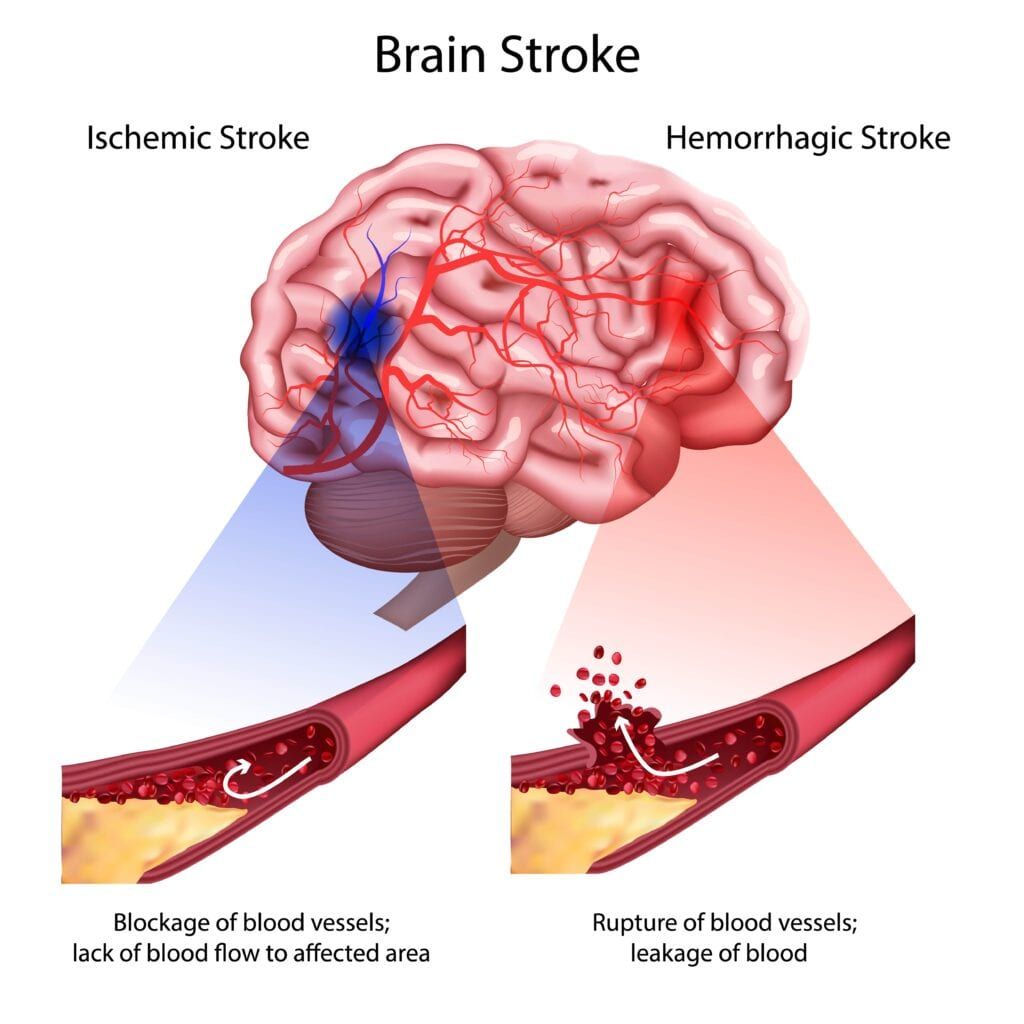
Before discussing stroke-related headaches, it is important to first establish a firm understanding of what happens during a stroke. A stroke occurs when blood flow to the brain is interrupted. There are two types of strokes, including:
- Ischemic stroke: when an artery that supplies blood to the brain becomes blocked and causes brain cell death
- Hemorrhagic stroke: when an artery in the brain bursts, causing bleeding in the brain
When it comes to recognizing a stroke, the acronym FAST is used by the American Stroke Association. This acronym stands for the main symptoms associated with early signs of a stroke, such as:
- F: facial drooping on one side of the face
- A: arm weakness
- S: slurred speech or speech difficulty
- T: time to call emergency services
Stroke-Related Headaches
In addition to the classic stroke symptoms associated with the FAST acronym, around 7-65% of people undergoing a stroke will experience some form of a headache. People describe a stroke-related headache as a very severe headache that comes on within seconds or minutes. Oftentimes, the area affected by the headache is directly related to where the stroke occurs. For example, a blocked carotid artery can cause a headache on the forehead, while a blockage towards the back of the brain can cause a headache towards the back of the head. This ultimately means that there is not one headache location that signals a stroke, since they can occur anywhere on the head.

In some cases, it may be hard to tell the difference between a migraine and a stroke-related headache. This is because both migraines and stroke-related headaches have some overlapping symptoms such as: disorientation, a general feeling of being unwell, changes in vision, and vertigo. The easiest way to differentiate between the two is to pay attention to sensations. A migraine headache produces sensations like auras, flashing lights, or tingling skin, while a stroke-related headache causes sensations to be lost, such as a loss of vision or feeling. Additionally, migraine headaches are caused by recognizable triggers and the pain is described as a throbbing that gets gradually worse, while strokes can happen at random and cause pain that is sudden and severe.
A “mini stroke” can also cause a stroke-related headache. Mini strokes are more formally known as transient ischemic attacks characterized by a temporary interruption of blood flow. Unlike a stroke, with a TIA the brain tissue is only temporarily damaged and recovers once blood flow has been restored. Still, TIAs produce identical symptoms to a stroke, however the symptoms can last anywhere from only 5 minutes to 24 hours. Although the symptoms can be short-lived, a TIA should be treated like a stroke, since they are often a warning sign to a full-blown stroke. Seeking treatment early can prevent a stroke, as well as permanent brain damage.

Dr. Kashouty, a diplomate of the American Board of Psychiatry and Neurology (ABPN), practices general neurology with fellowship trained specialization in clinical neurophysiology. Dr. Kashouty finds the form and function of the nerves and muscles the most interesting part of neurology, which is what led him to specialize in neurophysiology with more emphasis on neuromuscular conditions. He treats all neurological diseases, but his main focus is to treat and manage headaches, movement disorders and neuromuscular diseases.