Strokes can strike like a bolt out of the blue, leaving devastation in their wake. Yet, while we count high blood pressure and heart disease as familiar foes in this battle, there are a myriad of other, less recognized factors silently shaping our stroke risk profile. From the air we breathe to the stress we shoulder, these covert culprits stealthily undermine our vascular health. This blog unveils some surprising stroke risk factors lurking in the shadows of everyday life—elements that don’t feature in our regular health checks but are just as potent in their capacity to harm. It’s time to cast a light on these hidden hazards and arm ourselves with the knowledge to counter their threat.
The Unexpected Culprits
Air Pollution:

Recent studies have highlighted a strong link between long-term exposure to air pollution and strokes. Invisible to the eye but pervasive in our environment, the pollutants emitted from vehicles, industrial processes, and the burning of fossil fuels consist of fine particulate matter that we inhale daily. These particles, especially those under 2.5 micrometers in diameter, are small enough to enter the bloodstream and incite a cascade of adverse effects. They can exacerbate inflammation within the body and accelerate the oxidation of blood vessels, impairing their function and contributing to the development of atherosclerosis—a leading cause of stroke. Long-term exposure to this silent menace has been linked to an increased incidence of strokes, as it disrupts the delicate balance of the cardiovascular system, emphasizing the need for stringent air quality regulations and protective measures for at-risk populations.
Sleep Disorders:
Sleep apnea and other sleep disorders present a hidden stroke risk factor, often overlooked yet critically impactful. Sleep apnea, characterized by repeated interruptions in breathing throughout the night, leads to fragmented sleep patterns and dramatic drops in blood oxygen levels. This nocturnal struggle for oxygen places immense stress on the cardiovascular system, causing fluctuating blood pressure and heart rhythm irregularities known as arrhythmias, both of which are prime conditions for a stroke. Moreover, the resultant poor sleep quality and chronic sleep deprivation can trigger inflammatory processes and impair glucose metabolism, further elevating stroke risk. As such, undiagnosed or untreated sleep disorders not only compromise the quality of life but also significantly raise the likelihood of cerebrovascular incidents, making it imperative for individuals with sleep disturbances to seek timely medical evaluation and intervention.
Mental Health:
The intricate interplay between mental health and stroke risk is a field of growing research and concern. Mental health disorders such as depression, anxiety, and chronic stress are not only debilitating to one’s psychological well-being but also exert a physical toll that may manifest in increased stroke risk. Chronic stress, for instance, triggers the release of stress hormones like cortisol and adrenaline, which can raise blood pressure and heart rate, leading to wear and tear on the cardiovascular system. Depression and anxiety may also lead to unhealthy coping behaviors, such as a sedentary lifestyle, poor dietary choices, and smoking, which independently increase stroke risk. Furthermore, the physiological effects of these mental health challenges, including inflammation and changes in blood coagulation, add another layer of risk. Recognizing and treating mental health issues is therefore not only critical for psychological health but may also be a preventative measure against strokes.
Silent Risk Factors
Hormones:
Hormones, the body’s chemical messengers, play a subtle yet significant role in stroke risk, particularly through their influence on blood flow and clotting mechanisms. For instance, fluctuations in estrogen levels, which can occur as a result of pregnancy, menopause, or hormone replacement therapies, have been associated with changes in blood coagulability and vascular resilience. Women taking birth control pills or undergoing hormone treatments often face a slightly elevated stroke risk, especially if they smoke or have high blood pressure. Additionally, conditions like hyperthyroidism or Cushing’s syndrome that disrupt hormonal equilibrium can lead to hypertension and other metabolic changes, increasing stroke vulnerability. Even though these hormonal shifts are a natural part of life or necessary for some medical treatments, understanding their potential impact on stroke risk is crucial for informed healthcare decisions and preventive strategies.
Infection:
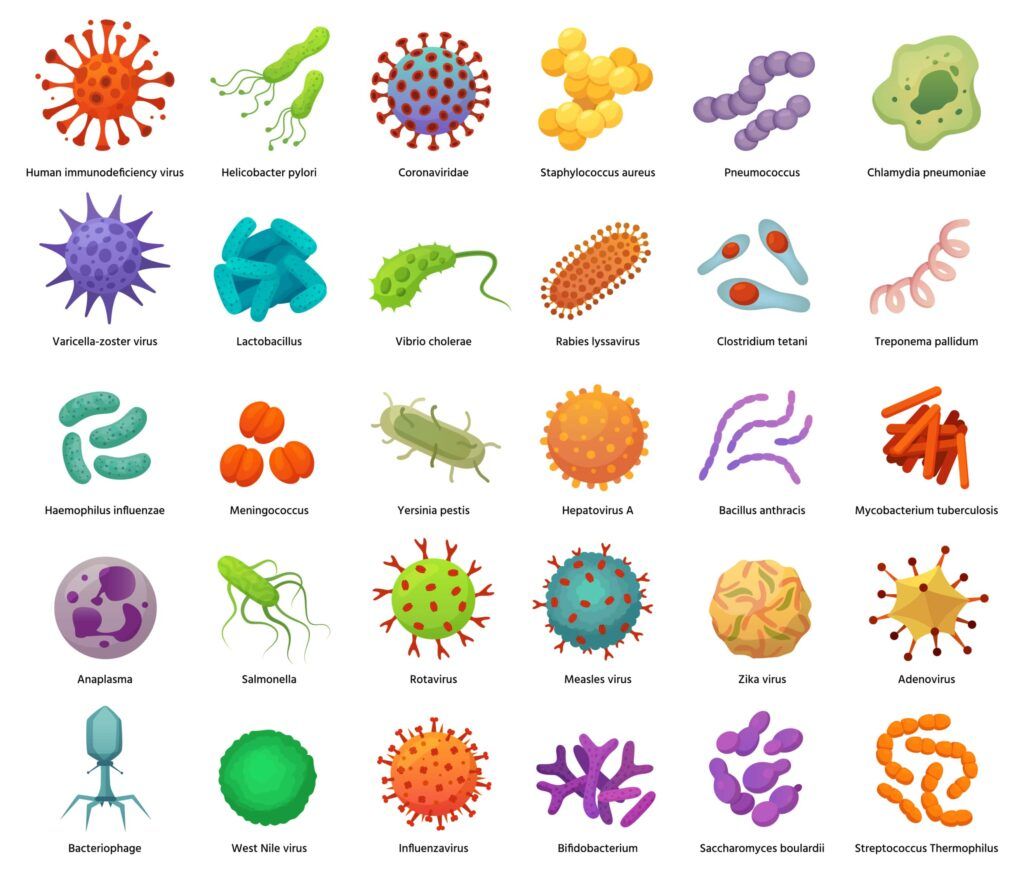
Specific infections, particularly those causing inflammation or endocarditis—where the heart’s inner lining is inflamed—can create conditions ripe for a stroke. The inflammation response triggered by infections can lead to the formation of blood clots, which can then travel to the brain, blocking vital blood vessels. Moreover, infections such as meningitis, characterized by inflammation of the protective membranes covering the brain and spinal cord, can narrow blood vessels, reducing cerebral blood flow and potentially causing a stroke. Periodontal disease, too, has been flagged as a contributor to stroke risk, with the chronic gum infection adding to the body’s inflammatory burden. It’s a sobering reminder of how systemic infections can have far-reaching effects on our health, extending beyond their immediate symptoms and leading to serious vascular events like stroke.
Genetic Predispositions:
Genetic predispositions play a critical yet often underestimated role in the risk of stroke. Certain inherited conditions can predispose individuals to blood clotting disorders such as Factor V Leiden or prothrombin gene mutation, which enhance the blood’s propensity to clot and can lead to ischemic strokes, the most common type of stroke. The genetic makeup of an individual can also influence other stroke-related factors such as hypertension, diabetes, and metabolic syndrome. Ethnicity adds another layer to this risk, with some groups, like African Americans, being more susceptible to stroke than others, due to a combination of genetic predisposition and health disparities. Moreover, a family history of stroke significantly raises an individual’s risk, suggesting a hereditary component in stroke susceptibility. Understanding these genetic factors is vital for early intervention and targeted prevention strategies, emphasizing the need for personalized medical approaches based on one’s genetic profile.
Lifestyle Factors You Didn’t Consider
Sedentary Lifestyle:
A sedentary lifestyle is a silent yet significant risk factor for stroke, independent of other habits such as exercise routines. Extended periods of inactivity, which are increasingly prevalent in modern, screen-centric lifestyles, can impair blood circulation and lead to the development of risk factors for stroke like hypertension, obesity, and high cholesterol. The lack of movement for hours on end can cause blood to pool in the legs, increasing the risk of clotting, which becomes perilous if a clot travels to the brain, resulting in an ischemic stroke. Additionally, a sedentary lifestyle is often associated with poor dietary choices and a higher likelihood of diabetes, further exacerbating the risk. This creates a compelling case for integrating more movement into daily routines, not just as a means of fitness but as a fundamental preventive strategy against stroke.
Social Isolation:

Social isolation has surfaced as a complex risk factor for stroke. The link between social isolation and stroke lies not just in the realm of emotional distress but also in its physiological implications. Isolated individuals are more prone to the stress that accompanies loneliness, which can elevate blood pressure and trigger inflammatory responses. These stress-related physiological changes are well-documented pathways that increase stroke risk. Moreover, those who are socially isolated are less likely to have strong support networks that encourage healthy lifestyle habits and more likely to engage in behaviors detrimental to health, such as smoking or physical inactivity. The absence of social support can also lead to delays in seeking medical help or non-adherence to treatment regimens, thereby worsening outcomes for those who suffer a stroke. As such, fostering social connections and community support can be seen as integral to stroke prevention and recovery.
Education and Socioeconomic Status:
Education and socioeconomic status (SES) are intertwined with stroke risk in ways that underscore the broader implications of social determinants of health. Individuals with lower levels of education often have higher stroke risks, a disparity attributed to gaps in health literacy, which affects the understanding of stroke symptoms and the importance of timely treatment. The implications of SES are multifaceted; lower income brackets often correlate with limited access to healthcare, higher exposure to stressors, and increased prevalence of unhealthy lifestyles due to economic constraints. These conditions can lead to unmanaged health issues such as hypertension, diabetes, and obesity, all stroke risk accelerants.
Conclusion
In conclusion, the tapestry of stroke risk factors is woven with a multitude of threads, some stark and some subtle. Beyond the well-publicized dangers of high blood pressure and poor dietary habits, lie underappreciated factors like air pollution, sleep disorders, mental health, hormonal fluctuations, infections, genetic predispositions, and the nuances of a sedentary lifestyle, social isolation, as well as education and socioeconomic status. Acknowledging the full spectrum of these risks is imperative for a comprehensive stroke prevention strategy. It encourages a more vigilant and inclusive approach to health, urging us to consider environmental, psychological, and societal factors that contribute to stroke incidence. By broadening our understanding and action against these diverse risk elements, we can better safeguard our communities and fortify our defenses against the devastating impact of strokes.

Dr. Kashouty, a diplomate of the American Board of Psychiatry and Neurology (ABPN), practices general neurology with fellowship trained specialization in clinical neurophysiology. Dr. Kashouty finds the form and function of the nerves and muscles the most interesting part of neurology, which is what led him to specialize in neurophysiology with more emphasis on neuromuscular conditions. He treats all neurological diseases, but his main focus is to treat and manage headaches, movement disorders and neuromuscular diseases.




