According to the Centers for Disease Control and Prevention (CDC), the number of people who have died from a drug overdose in 2021 has increased six times since 1999, with a 16% increase from 2020-2021 alone. Out of these deaths in 2021, 75% of drug overdose deaths involved an opioid. The opioid crisis has cast a shadow over public health, as these alarming statistics highlight its devastating impact on individuals and communities worldwide. As the search for effective treatment solutions intensifies, medical cannabis emerges as a potential ally in this battle. Despite its controversial legal status in various regions, there is growing interest in exploring how cannabis can be utilized to alleviate opioid dependence. This blog aims to delve into the role of medical cannabis in reducing opioid addiction, examining its efficacy, patient experiences, and the challenges it faces in the medical and legal landscapes. Through a comprehensive analysis, we will uncover whether medical cannabis can offer a viable alternative in the fight against the opioid epidemic.
In This Blog:
- Understanding Opioid Dependence
- Overview of Medical Cannabis
- Medical Cannabis and Pain Management
- Research on Medical Cannabis and Opioid Dependence
Understanding Opioid Dependence
Opioid dependence is a medical condition characterized by a compulsive need to use opioid drugs, even when they are no longer medically required. This dependency can develop from the prolonged use of opioids, including prescription pain relievers, heroin, and synthetic opioids such as fentanyl. The root causes of opioid addiction are multifaceted, involving factors such as chronic pain, psychological stress, and genetic predisposition, alongside environmental and social influences.

The mechanics of opioid dependence begin in the brain, where opioids bind to specific receptors, mitigating pain and releasing dopamine, a neurotransmitter associated with pleasure and reward. This process can lead to a euphoric sensation, encouraging repeated use and, over time, leading to neurological changes. These changes in brain chemistry can result in tolerance (needing more of the drug to achieve the same effect) and physical dependence, where the absence of the drug causes withdrawal symptoms.
The consequences of long-term opioid use are profound, affecting almost every aspect of an individual’s life. Physically, prolonged use can lead to a range of complications, from nausea and constipation to increased risk of overdose and death. Psychologically, it can cause mood disorders, cognitive impairment, and reduced quality of life. Socially, opioid dependence often leads to issues such as unemployment, relationship breakdowns, and financial instability.
In summary, opioid dependence is a complex disorder with significant health, social, and economic ramifications. Understanding the nature of this dependence is crucial for exploring alternative treatment methods, such as the use of medical cannabis, which could offer a safer and less addictive path for managing pain and reducing opioid use.
Overview of Medical Cannabis
The use of cannabis for medical purposes has a history that dates back thousands of years, with evidence of its use in ancient civilizations for a variety of ailments. Despite this long history, the legal status of medical cannabis has been contentious, with significant variations across different regions. In recent years, however, there has been a shift towards greater acceptance and legalization of medical cannabis in many parts of the world, driven by growing evidence of its therapeutic benefits.
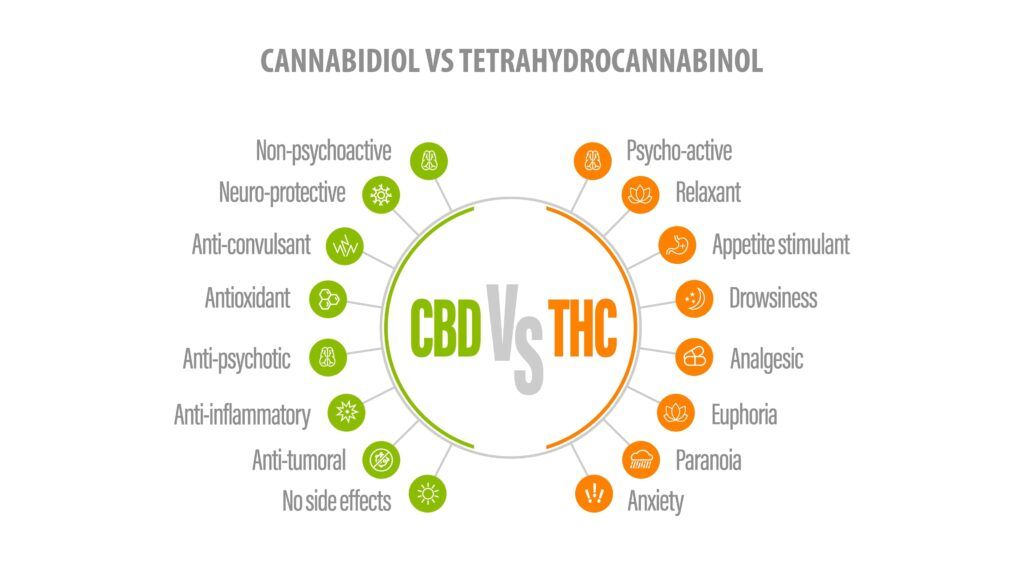
Medical cannabis refers to the use of the cannabis plant or its extracts to treat symptoms of illness and other conditions. The cannabis plant contains many compounds, but the two most significant for medical use are Tetrahydrocannabinol (THC) and Cannabidiol (CBD). THC is the psychoactive component that produces the “high” associated with cannabis use, while CBD is non-psychoactive and has been shown to have anti-inflammatory, analgesic, and anti-anxiety properties.
The therapeutic effects of cannabis are believed to be derived from its interaction with the body’s endocannabinoid system, a complex network of receptors and neurotransmitters that plays a key role in regulating various physiological processes, including pain sensation, mood, appetite, and memory. By interacting with this system, cannabis compounds can modulate these processes, providing relief from symptoms such as chronic pain, nausea, and anxiety, which are often associated with serious medical conditions.
Despite its potential, the use of medical cannabis is not without controversy. Concerns about the risk of addiction, mental health effects, and the lack of standardized dosing guidelines are among the issues that have hindered its widespread acceptance in the medical community. Nevertheless, as more research is conducted and public attitudes continue to evolve, medical cannabis is increasingly being considered as a viable option in the treatment of a range of conditions, including as an adjunct therapy for reducing opioid dependence.
Medical Cannabis and Pain Management
The use of medical cannabis in pain management represents a significant shift in the approach to treating chronic pain, an ailment that often leads to opioid prescription and, subsequently, potential dependence. Cannabis has been utilized for its analgesic properties since ancient times, and recent scientific studies have begun to shed light on how it can be used effectively to alleviate pain.
Medical cannabis can manage pain through its compounds, primarily THC and CBD, which interact with the body’s endocannabinoid system. This system plays a critical role in regulating pain perception. THC binds to cannabinoid receptors in the brain and nervous system, reducing pain and inflammation, but also producing euphoric effects. CBD, on the other hand, does not bind directly to these receptors but influences the body to use its own endocannabinoids more effectively, helping to reduce pain and inflammation without the psychoactive effects of THC.

Comparatively, medical cannabis offers a different mechanism of action than opioids, which bind to opioid receptors in the brain to block pain signals and release dopamine. This difference in action suggests that cannabis might be a less addictive alternative to opioids for pain management. Several studies have indicated that patients using medical cannabis for pain relief report significant reductions in their use of opioids, with some even discontinuing opioid use altogether.
Patient testimonials and case studies further support the potential of medical cannabis in pain management. Many patients who have switched from opioids to medical cannabis report better pain control, improved quality of life, and fewer side effects. However, it’s important to note that medical cannabis is not a one-size-fits-all solution and may not work for everyone. The effectiveness of medical cannabis for pain relief can vary depending on the individual, the type of pain, and the specific cannabis product used.
In summary, medical cannabis presents a promising alternative for pain management, with the potential to reduce the reliance on opioids. Its use is supported by historical evidence, contemporary research, and patient experiences, all pointing towards its ability to manage pain effectively and with fewer risks of addiction compared to opioids. However, further research is needed to fully understand its efficacy, optimal dosing, and long-term effects, ensuring that medical cannabis can be safely and effectively integrated into pain management practices.
Research on Medical Cannabis and Opioid Dependence
The intersection of medical cannabis and opioid dependence is a burgeoning field of research, fueled by the need to address the opioid crisis. Studies have increasingly focused on whether cannabis can be an effective tool in reducing opioid use and dependency. This section examines the existing research on the topic, the mechanisms behind cannabis’s potential effects on opioid dependence, and the limitations of current studies.
Summary of Key Studies
Research into the use of medical cannabis as a treatment for opioid dependence has yielded promising results, however more research is needed. One article reviewed nine studies aimed at evaluating the use of medical cannabis as an adjunct to opiates given to patients with non-cancer chronic pain. This article found that there was a 64-75% reduction in opioid dosage when used in combination with medical cannabis. While this study underscores the potential of medical cannabis (MC) to reduce opioid dosage in non-cancer chronic pain treatment, it cautions against making definitive conclusions due to the lack of causal evidence and established optimal dosages. It highlights the need for further research to understand the health implications of combining MC with opioids.
Another article evaluated Canadian medical cannabis patients over a six-month period who were using a combination of medical cannabis and opioid medications. This study found a 78% reduction in mean opioid reduction at the six month mark. This study offers a more individual-focused perspective, suggesting that cannabis may serve a harm reduction role in the opioid crisis by reducing opioid use and improving patients’ quality of life over six months, particularly for chronic pain management. Together, these studies suggest that while medical cannabis has potential benefits in reducing opioid dependence and enhancing life quality, more detailed and systematic research is necessary to fully comprehend its efficacy and safety in long-term pain management and its role in addressing the opioid crisis.
Mechanisms of Action
The potential of cannabis to reduce opioid dependence may be explained by its interaction with the body’s endocannabinoid system, which is involved in modulating pain, reward, and addictive behaviors. THC and CBD, the primary active compounds in cannabis, can affect the release of neurotransmitters and alter pain perception, potentially reducing the need for opioids. Furthermore, the euphoric effects of THC might substitute for those of opioids, helping to alleviate withdrawal symptoms and reduce cravings.
Limitations and Gaps in Research
While the initial findings are encouraging, there are several limitations to the current research on cannabis and opioid dependence. Many studies are observational and rely on self-reported data, which can be subject to bias and inaccuracies. There is also a lack of standardized dosing and formulations of cannabis, making it difficult to compare results across studies or establish optimal treatment protocols. Additionally, long-term studies are needed to understand the effects of sustained cannabis use, particularly concerning its potential for addiction and cognitive effects.
Conclusion
In conclusion, the exploration of medical cannabis as a potential solution for reducing opioid dependence is a promising avenue that warrants further investigation. While the current body of research provides encouraging signs of its efficacy and safety in pain management and opioid reduction, there are still many complexities to unravel, including optimal dosing, long-term effects, and legal considerations. The anecdotal and scientific evidence suggests that medical cannabis could offer a viable alternative to opioids, potentially leading to lower rates of addiction and overdose. However, comprehensive, controlled clinical trials are necessary to fully understand its role and efficacy in opioid dependence treatment. As we move forward, it is crucial for policymakers, healthcare providers, and researchers to collaborate in fostering an environment where the potential of medical cannabis can be fully explored and utilized to combat the opioid crisis, always prioritizing patient safety and public health.

Dr. Kashouty, a diplomate of the American Board of Psychiatry and Neurology (ABPN), practices general neurology with fellowship trained specialization in clinical neurophysiology. Dr. Kashouty finds the form and function of the nerves and muscles the most interesting part of neurology, which is what led him to specialize in neurophysiology with more emphasis on neuromuscular conditions. He treats all neurological diseases, but his main focus is to treat and manage headaches, movement disorders and neuromuscular diseases.




