Brain aneurysms, often undetected until they become life-threatening, pose a significant risk to neurological health. Understanding what brain aneurysms are, recognizing their signs, and knowing how to manage them is crucial. This blog aims to demystify brain aneurysms by exploring their prevention, detection, and management. We will delve into the causes and risk factors, discuss how lifestyle choices can influence prevention, outline the symptoms that warrant medical attention, and examine the treatment options available for managing this condition. By equipping readers with this knowledge, we aspire to foster proactive health behaviors and empower individuals to take charge of their neurological well-being.
In This Blog:
- Understanding Brain Aneurysms
- Prevention of Brain Aneurysms
- Detection of Brain Aneurysms
- Management of Brain Aneurysms
Understanding Brain Aneurysms
A brain aneurysm is a bulge or ballooning in a blood vessel in the brain. It can leak or rupture, causing bleeding into the brain (hemorrhagic stroke). Not all aneurysms burst, but the risk they pose makes understanding them critical. A brain aneurysm occurs when a weak spot in the wall of a brain artery bulges or balloons out. The pressure of blood flowing through the artery causes the weakened section to inflate. This potentially life-threatening condition can lead to severe outcomes if it ruptures, leading to a stroke, brain damage, or even death.
Types of Brain Aneurysms
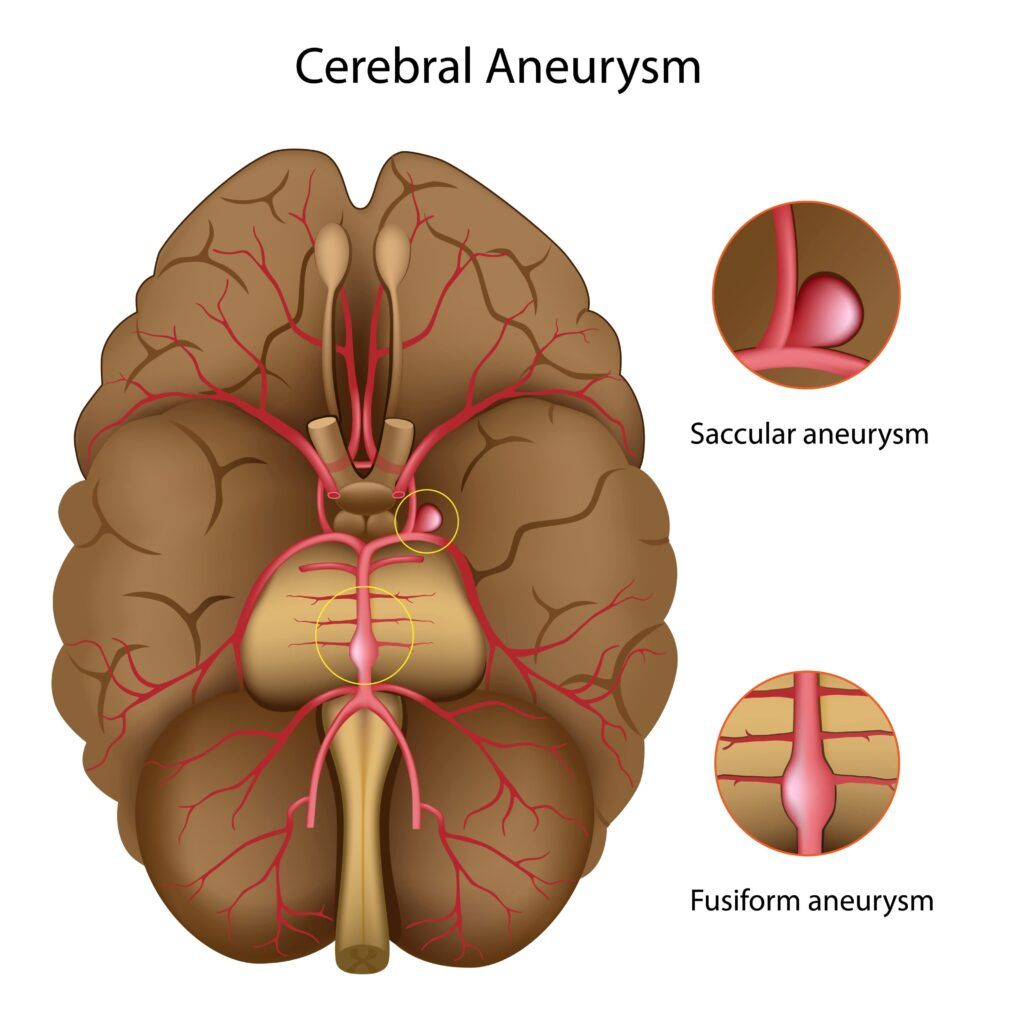
There are mainly three types of brain aneurysms:
- Saccular Aneurysms: Also known as “berry” aneurysms, these are the most common type, typically forming a sac-like bulge with a narrow neck connecting to the artery.
- Fusiform Aneurysms: These aneurysms involve the entire circumference of the vessel and do not have a distinct neck, bulging out in all directions.
- Dissecting Aneurysms: Caused by tears in the artery wall that allow blood to enter and split the layers of the wall, leading to a bulging section.
Causes and Risk Factors
The exact cause of brain aneurysms is often unclear, but several factors can increase the risk:
- Genetic predisposition: Family history of aneurysms can elevate the risk.
- High blood pressure: The increased pressure on blood vessel walls can lead to aneurysms.
- Smoking: Tobacco use significantly increases the risk.
- Age: The risk increases with age, particularly after 40.
- Gender: Women are more likely to develop brain aneurysms than men.
- Other conditions: Diseases like polycystic kidney disease, connective tissue disorders, and certain circulatory system issues can increase the likelihood of aneurysms.
Understanding brain aneurysms is the first step in managing them effectively. Knowledge of the types, causes, and risk factors associated with aneurysms can guide individuals in seeking appropriate medical advice and taking preventive measures.
Prevention of Brain Aneurysms
Preventing the development of brain aneurysms primarily involves managing risk factors and leading a healthy lifestyle. While not all aneurysms can be prevented, especially those due to genetic factors, certain lifestyle adjustments can reduce the risk.
Lifestyle Modifications
- Diet and Nutrition: A balanced diet rich in fruits, vegetables, whole grains, and lean proteins can help maintain healthy blood pressure and weight. Limiting the intake of saturated fats, cholesterol, and sodium is crucial to prevent arterial damage and high blood pressure, which can contribute to aneurysm formation.
- Exercise and Physical Activity: Regular physical activity helps maintain a healthy weight, reduce blood pressure, and strengthen the cardiovascular system. Engaging in moderate exercise for at least 150 minutes a week is recommended.
- Smoking Cessation and Alcohol Moderation: Smoking is a significant risk factor for aneurysms. Quitting smoking can drastically reduce the risk. Similarly, limiting alcohol consumption can prevent spikes in blood pressure that may contribute to aneurysm risks.
Managing Underlying Health Conditions

- Hypertension Control: High blood pressure is a leading cause of aneurysms. Regular monitoring and management of blood pressure through medication, diet, and lifestyle changes are essential.
- Diabetes Management: Keeping blood sugar levels under control helps prevent damage to blood vessels, reducing the risk of aneurysm formation.
- Treating High Cholesterol: High cholesterol can lead to atherosclerosis, which can weaken blood vessel walls and increase the risk of aneurysms. Managing cholesterol levels with diet, exercise, and medication is important.
Regular Check-ups and Screenings
For individuals at high risk, such as those with a family history of aneurysms or genetic conditions that increase risk, regular medical check-ups and screenings are vital. Imaging tests like MRI or CT scans can detect early aneurysms before they cause symptoms, allowing for timely intervention.
Prevention strategies for brain aneurysms are centered on reducing the known risk factors and leading a healthy lifestyle. By combining regular health screenings with proactive management of lifestyle and health conditions, individuals can significantly decrease their risk of developing an aneurysm.
Detection of Brain Aneurysms
Early detection of brain aneurysms is crucial for effective management and preventing serious complications. Recognizing the symptoms and undergoing the right diagnostic tests can lead to timely treatment, significantly reducing the risks associated with ruptured aneurysms.
Symptoms and Early Warning Signs
While many brain aneurysms remain asymptomatic until they rupture, certain signs and symptoms can indicate their presence:
- Severe headache: Often described as the “worst headache” ever experienced, it can be a sudden and severe symptom of a ruptured aneurysm.
- Vision changes: Blurred or double vision can occur if an aneurysm presses on the nerves controlling the eyes.
- Seizures: Aneurysms may cause seizures if they leak or rupture, affecting brain function.
- Other neurological symptoms: These can include stiffness in the neck, nausea, vomiting, sensitivity to light, or sudden changes in mental state or mood.
Diagnostic Methods
When a brain aneurysm is suspected, several diagnostic tests can be used to confirm its presence:
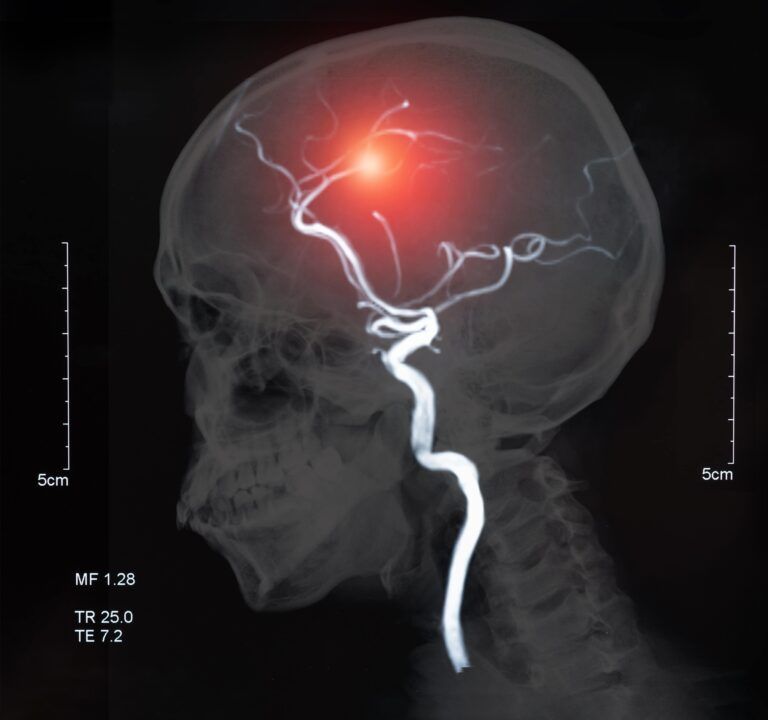
- Computed Tomography (CT) Scan: A CT scan of the head is often the first test performed when a ruptured aneurysm is suspected, as it can quickly detect bleeding in the brain.
- Magnetic Resonance Imaging (MRI): An MRI can provide detailed images of the brain and blood vessels, helping identify aneurysms before they rupture.
- Cerebral Angiography: This invasive procedure involves injecting a contrast dye into the brain’s blood vessels to provide clear images of blood flow and vessel structure, accurately identifying the size and shape of an aneurysm.
Importance of Early Detection
Detecting an aneurysm early can be life-saving. Early diagnosis allows for monitoring and potentially treating the aneurysm before it ruptures. For aneurysms that are small and not posing immediate risk, regular monitoring can help assess their growth and risk of rupture, guiding the need for preventive treatment.
Early detection of brain aneurysms is a critical component in preventing catastrophic outcomes. Being aware of the symptoms and undergoing timely and appropriate diagnostic tests can lead to early intervention and significantly better prognosis.
Management of Brain Aneurysms
Once a brain aneurysm is detected, managing it effectively is crucial to prevent rupture and ensure patient safety. Management strategies vary depending on the size, location, and risk of rupture of the aneurysm, as well as the patient’s overall health.
Monitoring and Conservative Management
For small aneurysms or those in less critical areas of the brain, conservative management, including regular monitoring, might be recommended. This approach often includes:
- Regular Imaging Tests: MRI or CT scans are conducted periodically to monitor the aneurysm’s size and growth rate.
- Managing Risk Factors: Patients are advised to control blood pressure, stop smoking, manage cholesterol levels, and maintain a healthy lifestyle to reduce the risk of aneurysm growth and rupture.
Surgical Interventions
In cases where the aneurysm is large or showing signs of growth or where the patient’s health profile indicates a higher risk of rupture, surgical intervention may be necessary:
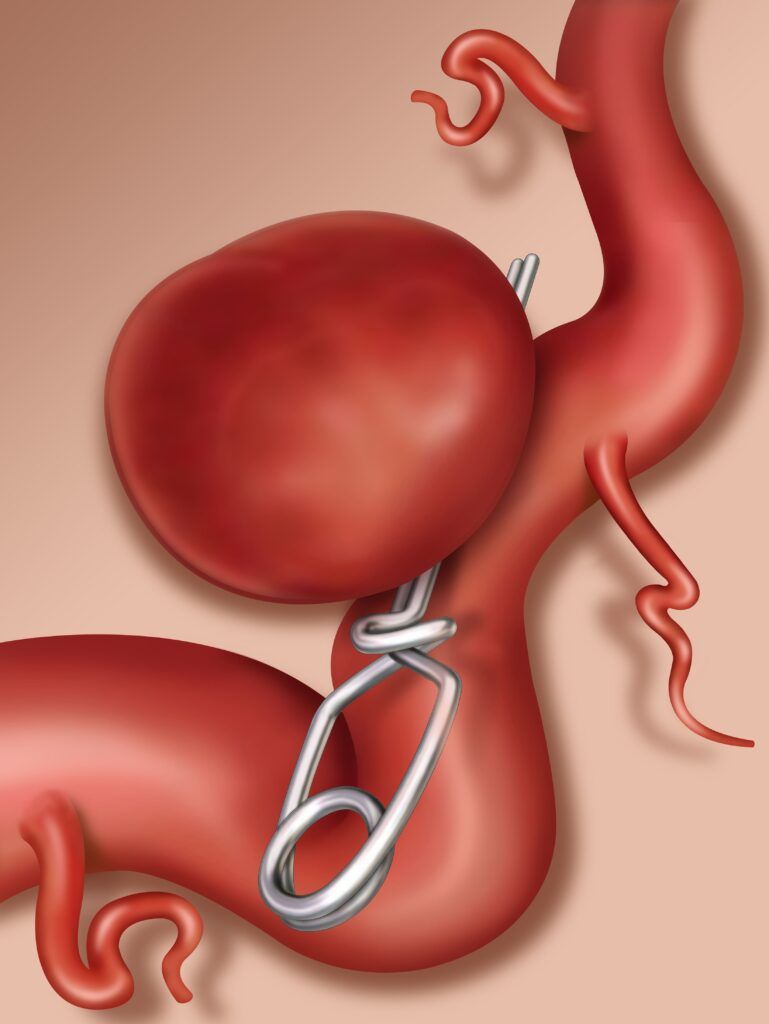
- Clipping: A small metal clip is placed at the base of the aneurysm to cut off the blood flow, preventing rupture. This surgery involves opening the skull and is considered invasive.
- Coiling: A less invasive procedure where coils are inserted through the arteries in a catheter from the groin up to the brain aneurysm. The coils induce clotting and thus prevent blood flow into the aneurysm, reducing the risk of rupture.
- Flow Diverter Devices: These are stent-like devices placed in the parent blood vessel to divert blood flow away from the aneurysm, promoting healing of the vessel wall and preventing the aneurysm from growing or rupturing.
Post-surgical Care and Rehabilitation
After surgical treatment, post-surgical care is essential for recovery and includes:
- Hospital Monitoring: Patients are closely monitored for changes in neurological status and complications in the immediate postoperative period.
- Rehabilitation: Some patients may need physical, occupational, or speech therapy to recover from any neurological deficits caused by the aneurysm or the treatment procedure.
- Follow-up Care: Regular follow-up visits with healthcare providers are crucial to monitor the patient’s neurological health and prevent future vascular events.
Managing brain aneurysms is a multifaceted approach that involves careful monitoring and, when necessary, surgical intervention to prevent rupture and subsequent complications. Individualized treatment plans, tailored to each patient’s specific condition and risks, are essential for effective management and positive outcomes.
Conclusion
In conclusion, understanding, detecting, and managing brain aneurysms are pivotal in mitigating the risks associated with this serious condition. Prevention through lifestyle choices and managing underlying health conditions can significantly reduce the likelihood of developing an aneurysm. Early detection through vigilant awareness of symptoms and timely diagnostic imaging can be life-saving, allowing for appropriate management strategies to be employed. Whether through monitoring, surgical intervention, or post-treatment care, the goal remains to prevent rupture and minimize neurological damage. By empowering individuals with knowledge and access to medical resources, we can improve outcomes for those affected by brain aneurysms and enhance overall neurological health.

Dr. Kashouty, a diplomate of the American Board of Psychiatry and Neurology (ABPN), practices general neurology with fellowship trained specialization in clinical neurophysiology. Dr. Kashouty finds the form and function of the nerves and muscles the most interesting part of neurology, which is what led him to specialize in neurophysiology with more emphasis on neuromuscular conditions. He treats all neurological diseases, but his main focus is to treat and manage headaches, movement disorders and neuromuscular diseases.