Chronic spinal pain and radiculopathy are conditions that can significantly impact one’s quality of life. While many people might first think of seeing an orthopedic specialist for spine-related issues, there’s a compelling case for consulting a neurologist. Let’s delve into the intricacies of these conditions and understand why a neurologist might be the best specialist to consult.
Understanding Chronic Spinal Pain
Chronic spinal pain is a persistent pain that lasts for more than three months. The pain can be continuous or intermittent and can range from a dull ache to sharp, shooting pains. It can arise from various causes, including degenerative disc disease, spinal stenosis, and spondylolisthesis, among others. Another potential cause of chronic spinal pain is radiculopathy.
What is Radiculopathy?
Spinal radiculopathy, commonly referred to simply as radiculopathy, is a condition where one or more nerves in the spine become compressed, irritated, or inflamed. This compression can lead to a variety of symptoms that manifest not only at the site of the compression but also along the path of the affected nerve.
The symptoms and affected areas depend on the location of the nerve root that’s compromised. Here are the different types of radiculopathy based on their location in the spine:
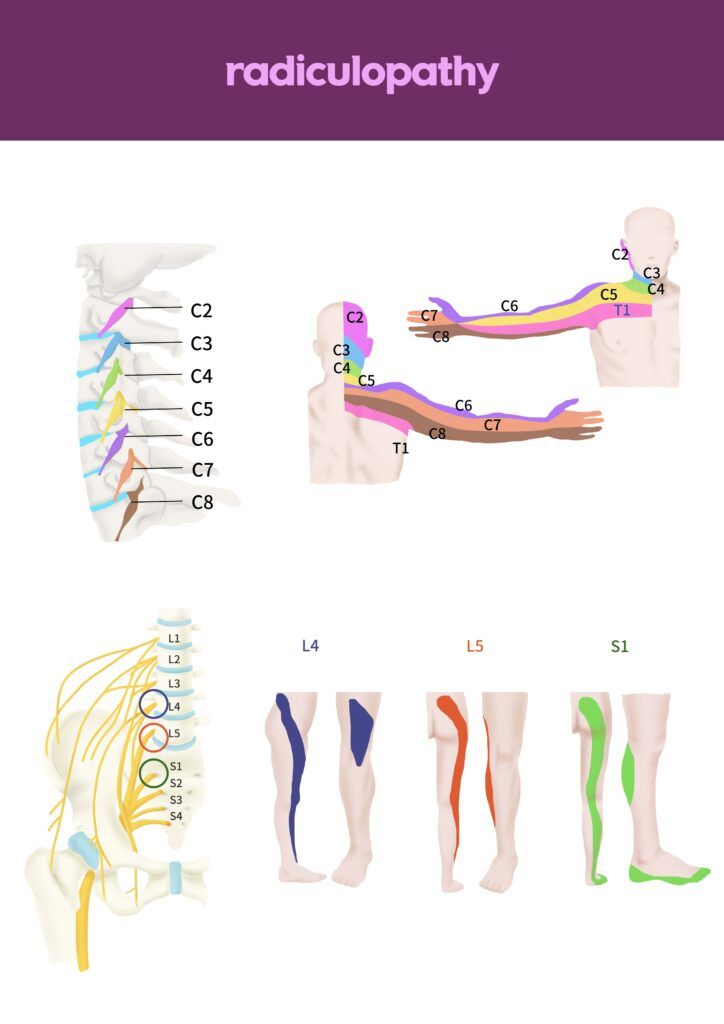
Cervical Radiculopathy (Neck)
- Location: Affects the cervical spine (neck region).
- Symptoms: Pain, numbness, tingling, or weakness that can radiate from the neck down into the shoulders, arms, hands, and fingers.
- Common Causes: Herniated discs, degenerative disc disease, and bone spurs in the cervical spine.
Thoracic Radiculopathy (Mid-Back)
- Location: Affects the thoracic spine (mid-back region).
- Symptoms: Less common than cervical or lumbar radiculopathy, it can cause pain in the chest, ribs, and sometimes the abdomen. The pain can be sharp, stabbing, or burning.
- Common Causes: Herniated discs, degenerative disc disease, and trauma in the thoracic region.
Lumbar Radiculopathy (Lower Back)
- Location: Affects the lumbar spine (lower back region).
- Symptoms: Often referred to as sciatica when the sciatic nerve is affected. Symptoms include pain, numbness, tingling, or weakness that radiates from the lower back into the buttocks, thighs, legs, and feet.
- Common Causes: Herniated discs, spinal stenosis, and spondylolisthesis in the lumbar region.
Why See a Neurologist?
Seeing a neurologist for chronic spine pain is crucial for several reasons:
Expertise in Nervous System Disorders:
The spine is not just a structural entity; it’s an integral part of the nervous system. Neurologists specialize in diagnosing and treating conditions of the nervous system, making them well-equipped to address issues related to spinal nerve roots and the spinal cord.
Comprehensive Diagnostic Capabilities:
Neurologists have access to and are trained in specialized tests like nerve conduction studies, electromyography, and advanced imaging techniques. These tests can pinpoint the exact cause of spine-related symptoms, ensuring a more accurate diagnosis.
Holistic Treatment Approach:
While pain management is essential, neurologists also focus on treating the underlying cause of the pain. This might involve medications, physical therapy, or even referrals for surgical interventions if needed.
Understanding of Related Conditions:
Chronic spinal pain can sometimes be a symptom of more severe neurological conditions, such as multiple sclerosis, tumors, or degenerative neurological disorders. Neurologists can identify these underlying conditions and ensure appropriate treatment.
Neurological Symptom Recognition:
Symptoms like numbness, tingling, muscle weakness, or coordination problems can be indicative of a neurological issue. A neurologist can differentiate between musculoskeletal and neurological causes of pain.
Personalized Treatment Plans:
Based on the specific diagnosis and the patient’s overall neurological health, neurologists can create tailored treatment plans that address both the pain and any associated neurological symptoms.
In essence, while orthopedic specialists play a vital role in managing certain spinal conditions, the potential neurological implications of chronic spinal pain make neurologists a valuable resource in the diagnostic and treatment process.
How Neurologists Diagnose Radiculopathy
Neurologists employ a combination of clinical evaluations, patient history, and specialized tests to diagnose radiculopathy. Here’s a step-by-step breakdown of the diagnostic process:
Patient History:
The neurologist will begin by taking a detailed history of the patient’s symptoms, including the onset, duration, nature of pain, and any factors that exacerbate or alleviate the pain. They’ll also inquire about any previous injuries, surgeries, or relevant medical conditions.
Physical Examination:
- Neurological Examination: The neurologist will assess muscle strength, reflexes, and sensory functions in specific areas of the body to identify any neurological deficits.
- Spurling’s Test: For suspected cervical radiculopathy, the neurologist might use this test, which involves tilting the head to the side and applying gentle pressure to see if it exacerbates the pain.
- Straight Leg Raise Test: For suspected lumbar radiculopathy, this test involves raising the patient’s leg while they lie flat. Pain during this movement can indicate sciatic nerve involvement.
Imaging Studies:
- Magnetic Resonance Imaging (MRI): Provides detailed images of the spine and can reveal herniated discs, spinal stenosis, tumors, or other abnormalities that might be compressing nerve roots.
- Computed Tomography (CT) Scan: Offers cross-sectional images of the spine and can be useful in detecting bone spurs or other bony abnormalities.
- X-rays: While they don’t show soft tissues like discs, they can reveal spinal alignment issues, fractures, or osteoarthritis.

Electrodiagnostic Studies:
- Electromyography (EMG): Measures the electrical activity of muscles. An abnormal EMG can confirm nerve damage and its source.
- Nerve Conduction Velocity (NCV): Assesses how fast electrical signals move through a nerve. Slowed conduction can indicate nerve compression.
Selective Nerve Root Blocks:
After gathering all the relevant information and test results, the neurologist will make a definitive diagnosis and recommend an appropriate treatment plan. It’s essential to have a comprehensive evaluation, as accurate diagnosis is crucial for effective treatment.
Discography:
A dye is injected into a spinal disc, and an X-ray or CT scan is taken. If this reproduces the patient’s pain and shows disc abnormalities, it can help pinpoint the affected disc.
After gathering all the relevant information and test results, the neurologist will make a definitive diagnosis and recommend an appropriate treatment plan. It’s essential to have a comprehensive evaluation, as accurate diagnosis is crucial for effective treatment.
Treatments for Radiculopathy
Neurologists approach the treatment of radiculopathy with a combination of conservative and interventional methods, depending on the severity and cause of the condition. Here’s an overview of the treatment strategies they might employ:
Conservative Treatments:
- Medications:
- Pain Relievers: Over-the-counter pain medications like acetaminophen or NSAIDs (e.g., ibuprofen) can help alleviate pain.
- Corticosteroids: Oral steroids or epidural steroid injections can reduce inflammation and pain.
- Muscle Relaxants: These can help with muscle spasms that sometimes accompany radiculopathy.
- Neuropathic Agents: Drugs like gabapentin or pregabalin can be effective for nerve pain.
- Physical Therapy: A physical therapist can guide patients through exercises to strengthen and stretch the affected area, improve posture, and promote healing. They may also use modalities like ultrasound or electrical stimulation to reduce pain.
- Activity Modification: Avoiding activities that exacerbate symptoms and adopting ergonomic practices can help in managing pain.
Interventional Procedures:
- Epidural Steroid Injections: These are injections of corticosteroids into the epidural space around the spinal cord. They can reduce inflammation and provide temporary relief from pain.
- Selective Nerve Root Blocks: An anesthetic is injected near the affected nerve root to block pain signals.
- Radiofrequency Ablation: This procedure uses heat to disrupt nerve function, reducing pain signals from the affected nerve.
Surgical Interventions:
If conservative treatments don’t provide relief or if the nerve compression is severe, a neurologist might refer the patient to a neurosurgeon for surgical evaluation. Potential surgeries include:
- Discectomy: Removal of the portion of a herniated disc that’s pressing on a nerve.
- Laminectomy or Laminotomy: Removal of part or all of the vertebral bone (lamina) to relieve pressure on the spinal cord or nerves.
- Spinal Fusion: Joining two or more vertebrae together to stabilize the spine.
- Artificial Disc Replacement: Replacing a damaged disc with an artificial one.
Alternative Therapies:
- Acupuncture: Some patients find relief from radiculopathy symptoms through acupuncture.
- Chiropractic Care: Spinal adjustments by a chiropractor might help in certain cases.
Lifestyle Recommendations:
- Weight Management: Maintaining a healthy weight can reduce strain on the spine.
- Regular Exercise: Strengthening core and back muscles can provide better support to the spine.
It’s essential to note that the best treatment approach depends on the specific cause, location, and severity of the radiculopathy. A comprehensive evaluation by a neurologist ensures that the treatment plan is tailored to the individual’s needs.
In Conclusion
While orthopedic specialists play a vital role in managing spinal conditions, the neurological implications of chronic spinal pain and radiculopathy make neurologists uniquely qualified to handle these issues. If you or someone you know is experiencing persistent spinal pain or symptoms suggestive of radiculopathy, consider consulting a neurologist for a comprehensive evaluation and holistic treatment approach. Your spine is not just about bones and muscles; it’s a vital part of your nervous system, and it deserves the best care possible.

Dr. Kashouty, a diplomate of the American Board of Psychiatry and Neurology (ABPN), practices general neurology with fellowship trained specialization in clinical neurophysiology. Dr. Kashouty finds the form and function of the nerves and muscles the most interesting part of neurology, which is what led him to specialize in neurophysiology with more emphasis on neuromuscular conditions. He treats all neurological diseases, but his main focus is to treat and manage headaches, movement disorders and neuromuscular diseases.




