The last section in the COVID-19 and the Brain article took a brief look at recent research being conducted on this relationship. In this section, we will begin looking at how COVID-19 can reach the brain by first taking a closer look at the virus itself and then evaluating how the virus enters the body.
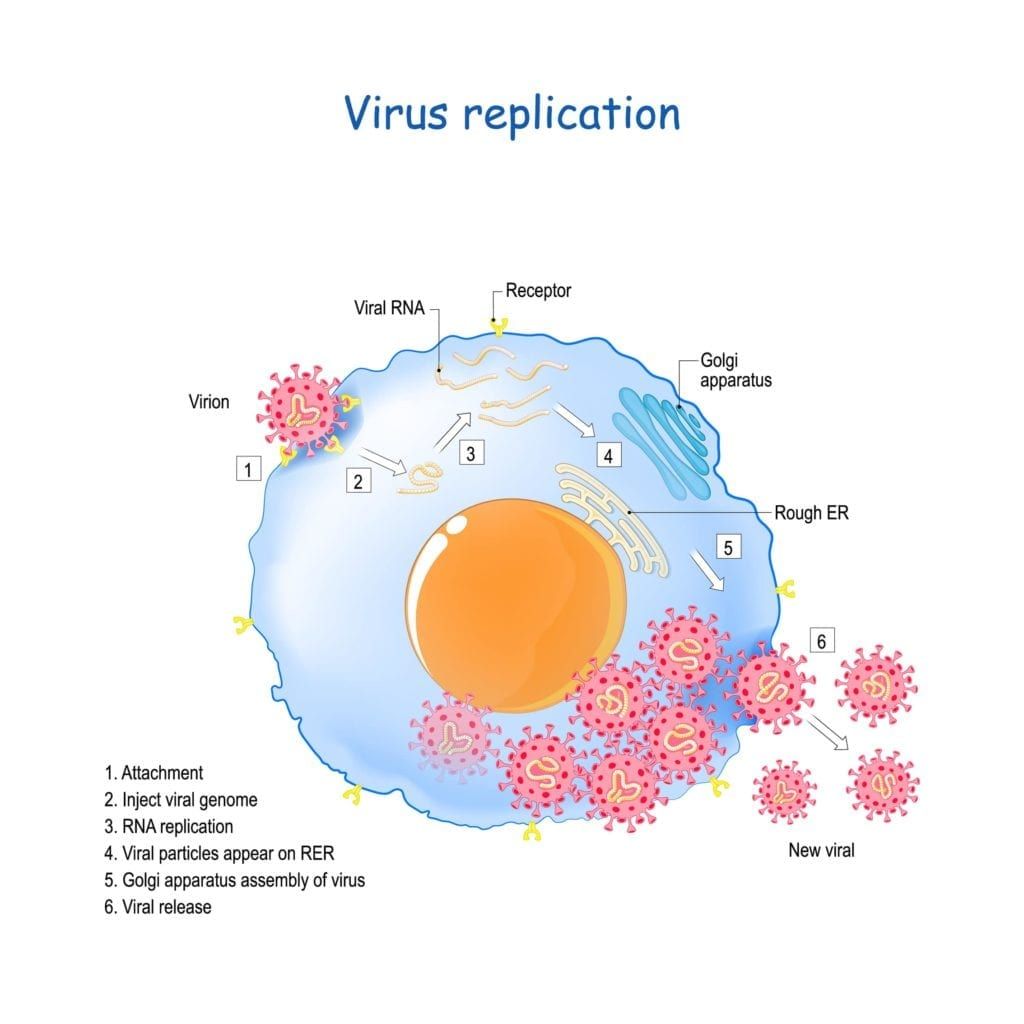
For starters, COVID-19 stands for coronavirus disease 2019 and is the name of the disease caused by the virion SARS-CoV-2. On its own, SARS-CoV-2 is ineffective, however it becomes a virus once it infects a healthy cell. The virion can come into contact with healthy cells when it enters the body through inhalation or touching infected surfaces. Since SARS-CoV-2 is an enveloped virus, it is also able to “hide” from the body’s natural defenses.
Once inside the body, the SARS-CoV-2 virion uses its spiky outer proteins to attach itself to ACE2 receptors found on the surface of healthy cells. ACE2 receptors play a role in several biochemical pathways that allow for wound healing, blood pressure, and inflammation. Only certain cells have ACE2 receptors and they are primarily found in the lower airway, with some being present in the nasal passages and mouth. The location of these receptors is why COVID primarily affects the respiratory system. However, ACE2 receptors are also found in the epithelial cells that line tissues and protective barriers within the lungs, heart, blood vessels, kidneys, liver, and GI tract.
SARS-CoV-2 is an RNA virus, meaning that it will attach itself to the external membrane of the host cell (through the ACE2 receptor) and then release a viral genome into the cell’s cytoplasm. This viral DNA will be transformed into messenger RNA (mRNA) where it will be used by the cell to create special enzymes for viral replication, create structural proteins to make new virions, and inhibit host cell DNA, RNA, and protein synthesis. Basically, this means that the SARS-CoV-2 virus eliminates natural cell functioning and instead uses the cell to make more copies of itself.
As the virus infects the cell, this reduces the function of ACE2 receptors, while also alerting the cell membrane of the viral presence. This activates the immune system and causes inflammation in the area where the infection is present. Since ACE2 receptors are found in the endothelial cells of blood vessels, this can cause inflammation to occur within the blood vessels, causing them to constrict. Prolonged periods of hyperinflammation combined with the inflammation of blood vessels can disrupt the blood-brain barrier.
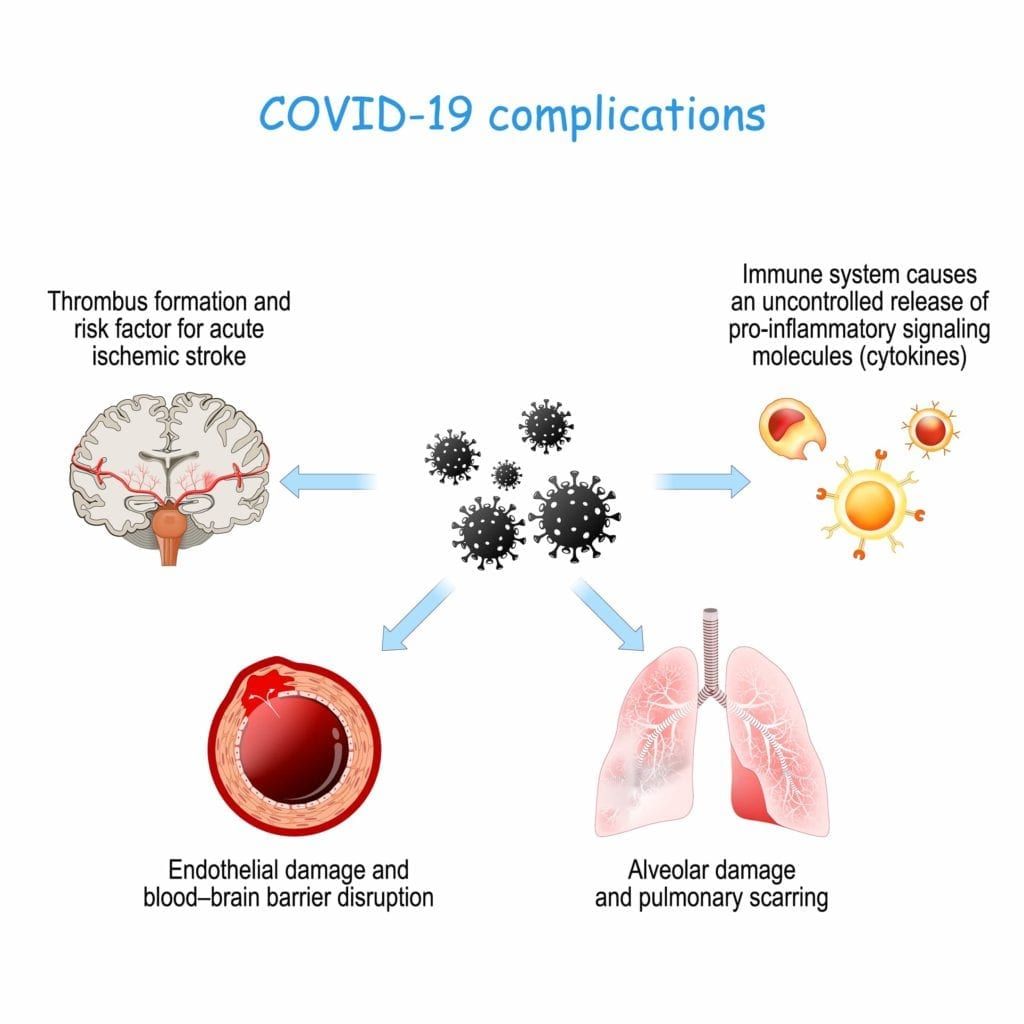
The blood-brain barrier is composed of semi-permeable endothelial cells that regulate the entrance of certain molecules into the central nervous system by passive diffusion. Simply stated, the blood-brain barrier protects the brain from damage by preventing the blood that circulates throughout the body (and carries pathogens) to freely enter the central nervous system. Unfortunately, the inflammation associated with ACE2 receptors and blood vessels makes the blood-brain barrier more permeable.
Not only does this make the blood barrier more permeable, it can also initiate an extreme immune system response known as a cytokine storm. Cytokines are immune system proteins that start to attack the body’s own cells when they are released in large amounts. In some cases, these immune system proteins may be able to pass through the blood-brain barrier and enter the central nervous system. This can also cause a hypercoagulable state, meaning that the risk of blood clots increases significantly. Not only that, but hypercoagulation also increases the risk of ischemic stroke.
In “Neuropathology of Patients with COVID-19 in Germany: A Post-Mortem Case Series”, researchers found that about 14% of patients who died from COVID showed ischemic lesions in the brain. Furthermore, they also found high levels of cytokines in the brainstem, cerebellum, and meninges that enclose the brain and spinal cord. SARS-CoV-2 viral proteins were also found in the cranial nerves that stemmed from the lower brain stem. While the study does not attribute neuropathological changes to the presence of SARS-CoV-2 in the CNS, it does note that the virus can be found in the brain and nerves. The researchers in this study stated that SARS-CoV-2 was able to enter the brain through the ACE2 receptors found on oligodendrocyte cells.
NOTE: This is Part II of IV. Other sections include:
- Part I: What Neurologists are Saying: An Introduction to Current Research
- Part III: The Neurological Symptoms of COVID-19
- Part IV: Post-COVID 19 Neurological Syndrome (PCNS)

Dr. Kashouty, a diplomate of the American Board of Psychiatry and Neurology (ABPN), practices general neurology with fellowship trained specialization in clinical neurophysiology. Dr. Kashouty finds the form and function of the nerves and muscles the most interesting part of neurology, which is what led him to specialize in neurophysiology with more emphasis on neuromuscular conditions. He treats all neurological diseases, but his main focus is to treat and manage headaches, movement disorders and neuromuscular diseases.