Guillain-Barré Syndrome (GBS) is a rare, potentially life-threatening condition that attacks the peripheral nervous system, often leading to rapid-onset muscle weakness and paralysis. While it remains relatively uncommon, understanding GBS is crucial due to its dramatic impact and the urgent need for medical intervention when symptoms arise. This blog post delves into the causes, symptoms, and treatment options for GBS, providing vital information for those diagnosed with the syndrome, healthcare professionals, and the general public. By exploring how this autoimmune response can be triggered by something as common as a minor infection, and discussing the available treatments and recovery prospects, this post aims to demystify GBS and offer hope and support to those affected.
In This Blog:
- What is Guillain-Barré Syndrome?
- Causes of Guillain-Barré Syndrome
- Symptoms of Guillain-Barré Syndrome
- Diagnosing Guillain-Barré Syndrome
- Treatment Options for Guillain-Barré Syndrome
What is Guillain-Barré Syndrome?
Guillain-Barré Syndrome (GBS) is a serious neurological disorder in which the body’s immune system mistakenly attacks part of its peripheral nervous system—the network of nerves located outside of the brain and spinal cord. This can lead to widespread inflammation and damage, causing muscle weakness, loss of reflexes, and even paralysis.
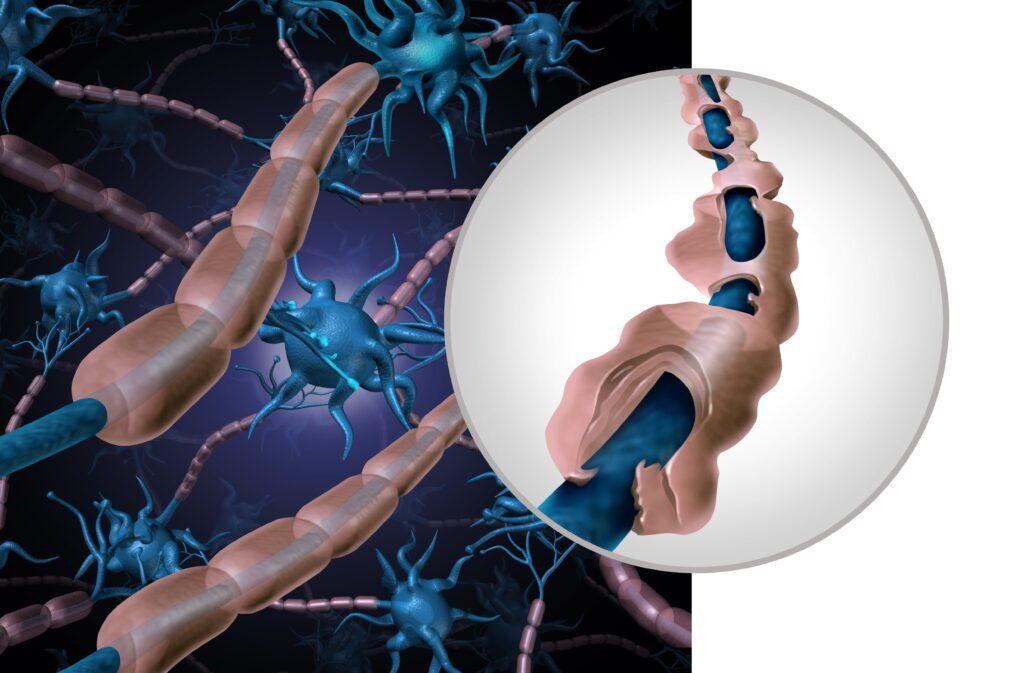
The exact mechanism of this autoimmune attack is not entirely understood, but it is known to disrupt the normal function of the nerves. Normally, nerves are covered in a protective sheathing called myelin, which facilitates the rapid transmission of electrical signals throughout the body. In GBS, the immune system begins to strip away this myelin sheath, a process known as demyelination, which results in the slowing or halting of nerve signal transmission. This damage can also affect the axons (the long part of the nerve cell), further impairing the nerves’ ability to communicate with muscles.
The onset of Guillain-Barré Syndrome can be quite sudden and unexpected, and it often follows a minor infection, such as a respiratory or gastrointestinal viral infection. The syndrome can vary greatly in severity; in mild cases, only slight muscle weakness may be experienced, while severe cases can result in complete paralysis and become life-threatening, particularly if the respiratory muscles are affected or if there are complications such as blood clots or severe infections.
Understanding GBS is critical, not only for those affected by it but also for the wider medical community, as early recognition and treatment are crucial for improving outcomes and reducing the risk of long-term disability.
Causes of Guillain-Barré Syndrome
Guillain-Barré Syndrome (GBS) is primarily considered to be an autoimmune disorder, though its exact causes remain not fully understood. The autoimmune response associated with GBS is believed to be triggered by an initial event, most commonly an infection. The leading suspects include:
- Bacterial infections: A significant number of GBS cases occur following infection with Campylobacter jejuni, a bacterium commonly associated with food poisoning.
- Viral infections: Respiratory or gastrointestinal viral infections, such as those caused by influenza or Epstein-Barr virus, can precede the development of GBS.
- Vaccinations: Occasionally, vaccinations have been linked to GBS, although this is extremely rare and the risk of GBS from vaccines is much lower than the risk from the diseases they prevent.
Once triggered, the body’s immune system begins to mistakenly attack its own nerve cells, believing them to be foreign invaders. This misdirected immune response results in the degradation of the myelin sheath and even the axons themselves, leading to the varied symptoms of GBS.
Symptoms of Guillain-Barré Syndrome
The symptoms of Guillain-Barré Syndrome can progress rapidly, often worsening significantly within a few days or weeks. The primary symptoms include:

- Weakness and tingling: Patients often first notice a tingling sensation and weakness starting in the feet and legs, which can then ascend to the upper body and arms. In some cases, this can start in the arms or face.
- Paralysis: As the condition progresses, muscle weakness can evolve into paralysis. This can affect both sides of the body and, in severe cases, lead to a total body paralysis known as quadriplegia.
- Autonomic nervous system issues: GBS can affect parts of the nervous system that control blood pressure, heart rate, and other automatic body functions, leading to problems such as blood pressure fluctuations and heart rhythm abnormalities.
- Breathing difficulties: If the muscles that control breathing become weakened, ventilatory support may be needed to help the patient breathe.
- Pain: Despite the paralysis, pain is a common symptom and can be quite severe, especially in the back and legs.
The rapid progression of these symptoms is a hallmark of Guillain-Barré Syndrome and what makes it a medical emergency. The wide range of symptoms reflects the extent of nerve damage and can vary significantly from person to person, necessitating tailored approaches to diagnosis and management.
Diagnosing Guillain-Barré Syndrome
Diagnosing Guillain-Barré Syndrome (GBS) involves a combination of clinical assessment and specific diagnostic tests, as there is no single test that can definitively diagnose GBS. The process typically includes:
- Clinical examination: This is crucial for assessing the pattern of weakness, reflex loss, and the progression of symptoms. A detailed medical history is also taken to identify preceding infections or other potential triggers.
- Nerve conduction studies (NCS): These tests measure the speed and strength of electrical signals traveling through the nerves. In GBS, these signals are often slower or do not travel at all, indicating nerve damage.
- Lumbar puncture (spinal tap): This involves collecting and analyzing cerebrospinal fluid (CSF), which can show an elevated protein level with a normal white cell count, a combination suggestive of GBS.
- Blood tests: While not diagnostic for GBS, blood tests can help rule out other conditions and identify potential triggers such as recent infections.
- MRI scans: Although not routinely required, MRI can be helpful to rule out other conditions that might mimic GBS, such as spinal cord lesions.
The goal of these diagnostic efforts is to confirm the presence of GBS and rule out other conditions with similar symptoms, such as myasthenia gravis or multiple sclerosis.
Treatment Options for Guillain-Barré Syndrome
Once Guillain-Barré Syndrome is diagnosed, treatment is primarily supportive but also involves specific therapies aimed at reducing the severity and duration of the illness:

- Intravenous immunoglobulins (IVIG): This treatment involves infusions of antibodies that can help lessen the immune system’s attack on the nerve cells. It is as effective as plasma exchange and can be easier to administer.
- Plasma exchange (plasmapheresis): This process involves removing and replacing the blood plasma, which contains the antibodies attacking the nerves. Removing these antibodies can reduce symptoms and accelerate recovery.
- Supportive care: As GBS can affect breathing, blood pressure, and other body functions, supportive care in a hospital setting is crucial. This may include mechanical ventilation if there are breathing difficulties, pain management, and treatment of autonomic dysfunction.
- Rehabilitation: Once the acute phase of the illness is over, long-term rehabilitation becomes a key component of treatment. This includes physical therapy to strengthen muscles, occupational therapy to assist with daily activities, and sometimes speech therapy if swallowing or speaking has been affected.
These treatments are most effective when started as soon as possible after the onset of symptoms. The aim is to lessen the immune attack on the nervous system, support body functions while the patient recovers, and facilitate a return to as normal a life as possible.
Conclusion
In conclusion, Guillain-Barré Syndrome (GBS) is a complex autoimmune disorder that requires prompt medical attention due to its rapid progression and potential severity. Understanding the triggers, recognizing the symptoms early, and obtaining an accurate diagnosis are crucial steps towards managing this challenging condition. Treatments such as intravenous immunoglobulins and plasma exchange, alongside comprehensive supportive care, can significantly improve outcomes. With ongoing research and advancements in medical science, there is hope for even better treatment options in the future. For those affected by GBS, accessing reliable information and support networks is essential for navigating the recovery process and regaining quality of life.

Dr. Kashouty, a diplomate of the American Board of Psychiatry and Neurology (ABPN), practices general neurology with fellowship trained specialization in clinical neurophysiology. Dr. Kashouty finds the form and function of the nerves and muscles the most interesting part of neurology, which is what led him to specialize in neurophysiology with more emphasis on neuromuscular conditions. He treats all neurological diseases, but his main focus is to treat and manage headaches, movement disorders and neuromuscular diseases.