Headache disorders, often underestimated in their complexity, extend far beyond the realm of migraines, affecting millions worldwide and significantly impacting quality of life. While migraines are widely recognized, many are unaware of the myriad other headache types, each with unique characteristics, triggers, and treatments. This blog aims to shed light on these lesser-known headache disorders, debunking common misconceptions and emphasizing the importance of accurate diagnosis and tailored treatment plans. By exploring tension-type headaches, cluster headaches, and various secondary headaches, we aim to provide a comprehensive guide that not only educates but also empowers individuals to navigate their symptoms and seek appropriate care.
In This Blog:
- Common Misconceptions About Headaches
- Types of Headache Disorders
- Diagnosis of Headache Disorders
- Treatment and Management
- Medical Cannabis for Headache Treatment
Common Misconceptions About Headaches
Headaches are often brushed off as minor ailments, but the reality is that they can be debilitating and indicative of various underlying disorders. One of the most prevalent misconceptions is conflating all types of severe headaches with migraines. Migraines, characterized by intense, pulsating pain often accompanied by nausea, vomiting, and sensitivity to light and sound, are just one subset of headache disorders.
Many people mistakenly believe that the severity of the headache determines its classification. However, other factors, such as duration, frequency, location of pain, and accompanying symptoms, are critical in differentiating between headache types. For instance, a tension-type headache, the most common form of headache, typically presents as a constant, dull ache on both sides of the head, differing markedly from the unilateral, throbbing nature of migraines.
Another common misunderstanding is that all headaches can be treated similarly. While over-the-counter painkillers might suffice for occasional tension-type headaches, they are often ineffective for cluster headaches or secondary headaches arising from underlying health issues. These types require specific treatments that target the unique aspects of each condition.
The belief that headaches are a normal part of life and should be endured rather than treated is another misconception that can hinder effective management of headache disorders. This notion can prevent individuals from seeking medical advice and receiving appropriate care, leading to unnecessary suffering and a diminished quality of life.
Understanding the nuances of various headache disorders is crucial for effective management and treatment. Recognizing that headaches can be complex and multifaceted is the first step toward demystifying these conditions and advocating for a more informed approach to headache care.
Types of Headache Disorders
Headache disorders encompass a range of conditions, each with distinct characteristics and management strategies. Understanding these differences is crucial for effective treatment. Here we delve into several common types beyond migraines:
Tension-Type Headaches
Tension-type headaches are the most prevalent, affecting a significant portion of the population. They manifest as a dull, pressing pain on both sides of the head, often described as feeling like a tight band around the forehead. Unlike migraines, they are not typically accompanied by nausea or vomiting and are less likely to be aggravated by routine physical activity. Stress, poor posture, and lack of sleep are common triggers, making lifestyle adjustments an essential part of management.
Cluster Headaches
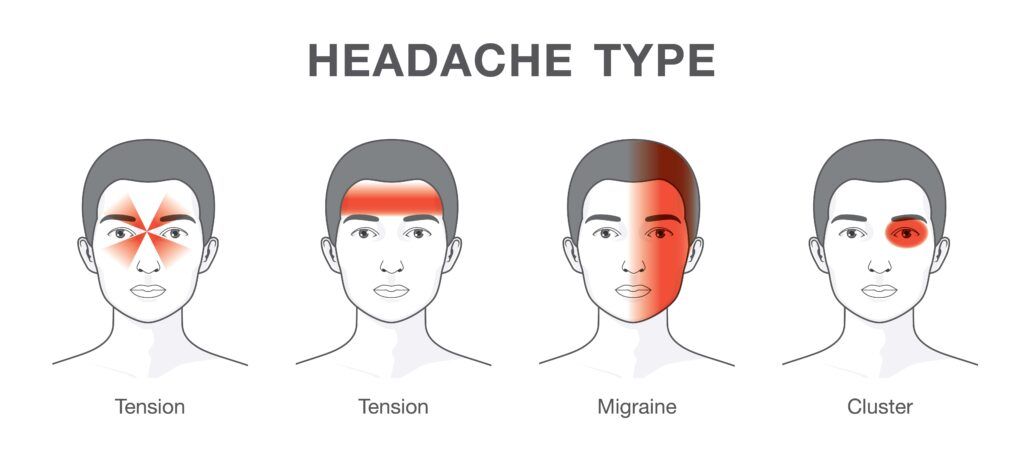
Cluster headaches are less common but far more severe. They are characterized by intense, piercing pain on one side of the head, often around the eye. These headaches occur in cyclical patterns or clusters, leading to frequent attacks over a period of weeks or months, followed by remission periods. The pain from a cluster headache is so severe that it is often described as one of the most painful conditions. Unlike migraines, cluster headaches can cause restlessness and agitation. Treatment typically includes fast-acting inhaled oxygen, triptans, and preventive medications to reduce the frequency and severity of attacks.
Secondary Headaches
Secondary headaches result from underlying medical conditions, such as sinus infections, brain tumors, or high blood pressure. These headaches vary widely in terms of severity, location, and accompanying symptoms, depending on the root cause. For example, a headache stemming from a sinus infection may present with facial pain and pressure, while a headache from a brain tumor might be persistent and worsen over time. Treating the underlying condition often resolves the headache, highlighting the importance of a thorough medical evaluation to identify and address the root cause.
Understanding the specific type of headache disorder is paramount in tailoring treatment and management approaches effectively. Each type demands a nuanced understanding to ensure that patients receive the most appropriate and effective care.
Diagnosis of Headache Disorders
Proper diagnosis is a critical step in the management of headache disorders, as it determines the most effective treatment plan. Diagnosing headache disorders involves a thorough evaluation of the patient’s medical history, symptoms, and sometimes, diagnostic tests. Here’s how the process typically unfolds:
Medical History and Symptom Assessment:
The first step in diagnosing a headache disorder is a detailed conversation about the patient’s medical history and a review of their symptoms. Patients are often asked about the nature, location, and duration of their headaches, as well as any accompanying symptoms such as nausea, light sensitivity, or visual disturbances. The frequency and intensity of the headaches, along with any identifiable triggers or patterns, are also crucial for diagnosis.
Physical and Neurological Examination:
After gathering medical history, a physical and neurological examination is conducted to check for signs of illness, infection, or neurological problems that could be causing the headaches. This may include checking for fever, stiff neck, mental confusion, weakness, or changes in vision, hearing, balance, and reflexes.
Diagnostic Tests:
While there are no specific tests to confirm many headache types like tension-type or cluster headaches, certain tests can be performed to rule out underlying conditions, especially if a secondary headache is suspected. Imaging tests like MRI or CT scans are used to look for abnormalities within the brain, such as tumors or signs of stroke. Other tests, such as blood tests, can help identify infections, toxic substances, or metabolic issues that might be contributing to the headache symptoms.
Specialist Referrals:
In some cases, especially when headaches are frequent, severe, or unresponsive to standard treatments, patients may be referred to a specialist. Neurologists, who specialize in brain and nervous system disorders, are often involved in the management of chronic or complex headache disorders.
Accurate diagnosis is essential for effective headache management. It enables healthcare professionals to recommend the most appropriate treatment strategies, which can vary significantly depending on the type and underlying cause of the headache. Therefore, individuals experiencing recurrent or severe headaches should seek medical attention to ensure an accurate diagnosis and appropriate treatment plan.
Treatment and Management
Effective treatment and management of headache disorders are tailored to the specific type of headache, its severity, frequency, and the individual’s overall health. Here’s how various headache disorders are typically addressed:
Tension-Type Headaches
- Lifestyle Changes and Home Remedies: Managing stress, improving posture, and ensuring regular sleep can significantly reduce the frequency of tension-type headaches. Relaxation techniques, such as yoga, meditation, and deep-breathing exercises, can also be beneficial.
- Medication: Over-the-counter pain relievers like ibuprofen, aspirin, or acetaminophen are commonly used. For chronic tension headaches, doctors may prescribe antidepressants or muscle relaxants to prevent headaches or reduce their frequency.
Cluster Headaches

- Acute Treatments: Fast-acting treatments are essential for cluster headaches due to their intense and sudden onset. Inhaled oxygen, triptan injections, or nasal sprays are often used to relieve pain quickly.
- Preventive Measures: To decrease the frequency and severity of cluster headache episodes, doctors may prescribe medications such as verapamil, corticosteroids, or lithium. Lifestyle adjustments and avoiding triggers like alcohol or strong smells can also help manage this condition.
Secondary Headaches
- Treating the Underlying Condition: The primary approach for secondary headaches is to treat the underlying cause, whether it’s an infection, high blood pressure, or a brain tumor. The specific treatment will depend on the diagnosed condition.
- Symptomatic Relief: While addressing the root cause, symptomatic treatments may be used to relieve headache pain. This could include pain relievers, anti-inflammatory drugs, or specific medications related to the underlying illness.
Specialist Consultations
For individuals with frequent, persistent, or particularly severe headaches, referral to a specialist like a neurologist might be necessary. Specialists can offer advanced treatment options, such as nerve blocks, physical therapy, or even surgery, in some cases.
Treatment plans for headache disorders often require a multifaceted approach, including both medical and non-medical strategies. Regular follow-ups and adjustments to the treatment plan are crucial, as they allow healthcare providers to monitor progress and make necessary changes. By adopting a comprehensive approach, individuals with headache disorders can achieve better control over their symptoms and improve their quality of life.
Medical Cannabis for Headache Disorder Treatment
The use of medical cannabis for treating headache disorders has gained attention due to its potential to alleviate pain and reduce the frequency of headache episodes. While research in this area is still evolving, some studies and anecdotal evidence suggest that cannabis may offer benefits for certain individuals suffering from chronic headaches, including migraines and cluster headaches. Here’s what is currently known about medical cannabis in the context of headache treatment:
Pain Relief:
Cannabis contains compounds like THC (tetrahydrocannabinol) and CBD (cannabidiol) that have pain-relieving properties. These compounds can interact with the body’s endocannabinoid system, which is involved in regulating pain, mood, and other physiological and cognitive processes. Some headache sufferers report that cannabis helps to reduce the intensity of headache pain.
Reduction in Frequency:
Preliminary studies suggest that regular use of cannabis may decrease the frequency of headache and migraine attacks in some patients. However, more extensive and controlled research is needed to validate these findings and understand the long-term effects.
Alternative to Traditional Medications:

For individuals who experience adverse side effects from standard headache medications, or for whom these medications are ineffective, medical cannabis may provide an alternative treatment option. However, it is crucial to consider the potential side effects of cannabis, including altered perception, mood changes, and cognitive impairment.
Legal and Medical Considerations:
The legality of medical cannabis varies by location, and it is important for patients to adhere to their region’s legal guidelines. Furthermore, patients should only use medical cannabis under the supervision of a healthcare provider who is knowledgeable about cannabis-related therapies and the specific headache disorder.
Need for Personalized Guidance:
As with any treatment, the effectiveness and appropriateness of medical cannabis will vary from person to person. Factors such as the type of headache, individual health conditions, and history of cannabis use can influence outcomes. Healthcare providers can help tailor treatment plans, including the selection of cannabis strains, dosages, and consumption methods, to meet individual needs.
While the potential of medical cannabis as a treatment for headache disorders is promising, it is essential to approach its use with caution and under medical guidance. Ongoing research and clinical trials are crucial for understanding the full scope of benefits and risks associated with cannabis use for headache disorders.
Conclusion
In conclusion, headache disorders encompass a diverse range of conditions, each with its unique characteristics and treatment requirements. Understanding the specific type of headache, whether it be tension-type, cluster, or secondary, is crucial for effective management and relief. With advancements in medical research, treatments have become more sophisticated, offering hope for those suffering from chronic and debilitating headaches. Alternative therapies, including medical cannabis, have also emerged as potential options, providing additional avenues for relief. It’s imperative for individuals experiencing persistent or severe headaches to seek professional medical advice to obtain an accurate diagnosis and an appropriate treatment plan. By doing so, they can not only alleviate their symptoms but also improve their overall quality of life, highlighting the importance of addressing headache disorders with the seriousness they deserve.

Dr. Kashouty, a diplomate of the American Board of Psychiatry and Neurology (ABPN), practices general neurology with fellowship trained specialization in clinical neurophysiology. Dr. Kashouty finds the form and function of the nerves and muscles the most interesting part of neurology, which is what led him to specialize in neurophysiology with more emphasis on neuromuscular conditions. He treats all neurological diseases, but his main focus is to treat and manage headaches, movement disorders and neuromuscular diseases.




