Muscles are essential components of our body, responsible for facilitating movement and maintaining posture. When problems arise within the muscle system, it can lead to a range of debilitating conditions. Two common categories of such disorders are myopathy and neuromuscular junction (NMJ) disorders. While both can affect muscle function, they differ in their origins, mechanisms, and clinical manifestations. In this blog, we will explore the similarities and differences between myopathy and neuromuscular junction disorders.
Myopathy: A Closer Look
Myopathy is a term used to describe a group of disorders characterized by abnormalities in muscle tissue, resulting in muscle dysfunction. These disorders primarily affect the skeletal muscles, which are the muscles that control voluntary movements, such as walking, lifting objects, and moving the limbs.
Myopathy can have various causes, including genetic mutations, autoimmune reactions, metabolic abnormalities, exposure to toxins or medications, and sometimes, the exact cause remains unknown (idiopathic). Here are some key characteristics and features of myopathy:
- Muscle Weakness: Myopathy typically leads to muscle weakness, which can range from mild to severe. This weakness often affects the proximal muscles, which are the muscles closer to the trunk of the body (e.g., hips, shoulders), making tasks like standing up from a seated position or lifting objects challenging.
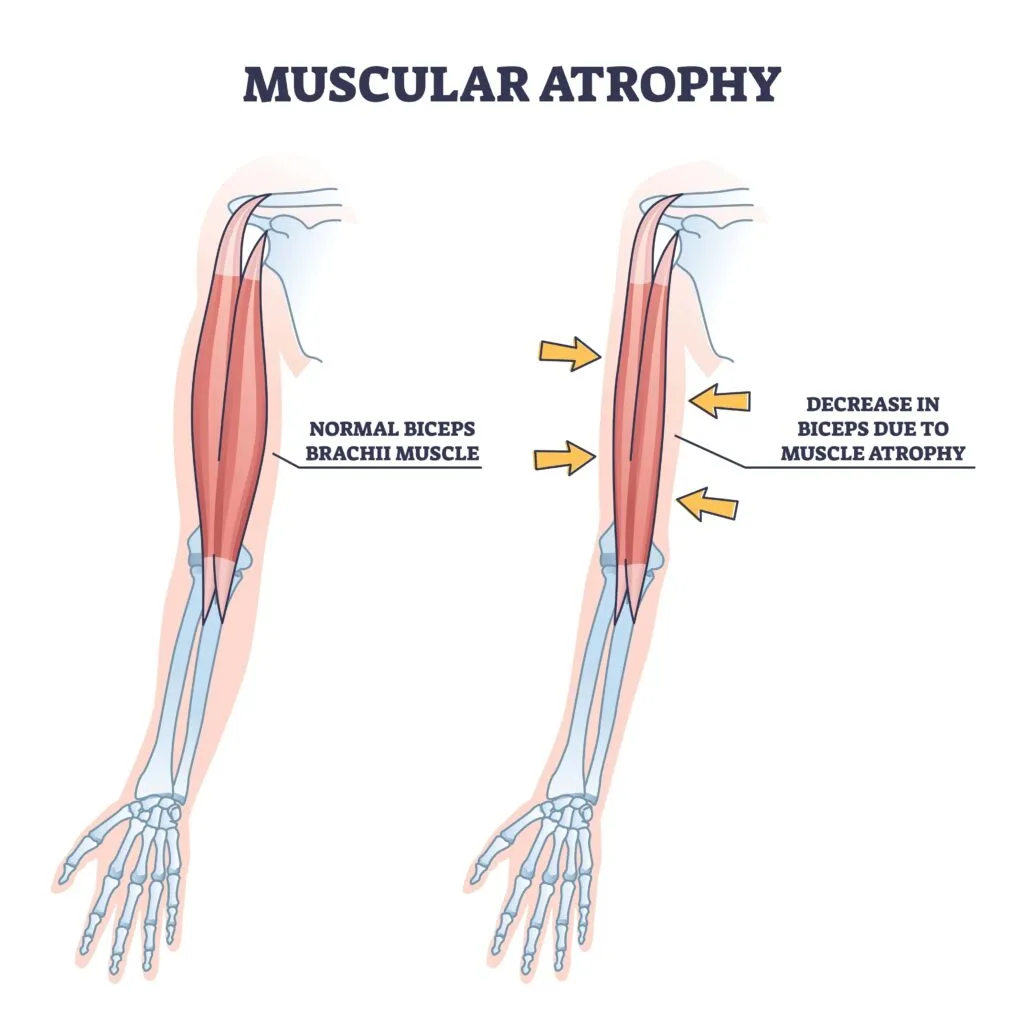
- Muscle Atrophy: In some cases, myopathy can cause muscle atrophy, which is the loss of muscle mass. As the muscles weaken and become less active, they may shrink over time.
- Muscle Pain and Fatigue: Individuals with myopathy may experience muscle pain and fatigue, especially with repetitive or sustained muscle use. These symptoms can limit physical activity.
- Difficulty with Mobility: Muscle weakness and fatigue can impair a person’s ability to perform daily activities, such as walking, climbing stairs, or even holding objects.
- Variable Presentation: Myopathy can present in various ways, and the severity of symptoms can vary widely from person to person. Some myopathies have a gradual onset, while others may develop suddenly.
Diagnostic Tests & Treatment:
To diagnose myopathy and determine its underlying cause, healthcare providers often use a combination of tests, including blood tests to assess muscle enzymes, electromyography (EMG) to evaluate muscle function, and muscle biopsy to examine muscle tissue at a cellular level. Genetic testing may also be necessary in some cases, especially when a hereditary form of myopathy is suspected.
Treatment for myopathy depends on the specific type and underlying cause of the disorder. Management may include physical therapy to maintain muscle strength and flexibility, medications to address symptoms or underlying conditions, lifestyle adjustments, and, in some cases, gene therapy or other specialized interventions.
There are numerous types of myopathies, each with its own unique characteristics and genetic or environmental causes. Some well-known myopathies include Duchenne muscular dystrophy, Becker muscular dystrophy, myotonic dystrophy, and inflammatory myopathies like polymyositis and dermatomyositis.
Neuromuscular Junction Disorders: A Brief Overview
Neuromuscular junction (NMJ) disorders are a group of medical conditions that primarily affect the neuromuscular junction, which is the specialized connection point between motor neurons (nerve cells) and skeletal muscle fibers. The neuromuscular junction plays a crucial role in transmitting nerve signals from the central nervous system to the muscles, leading to muscle contraction and movement. When there are disruptions at this junction, it can result in various neuromuscular problems.
NMJ disorders often manifest with muscle weakness and fatigue that worsens with muscle use. Unlike myopathies, NMJ disorders can display fluctuating symptoms, with weakness improving after rest. Electromyography (EMG) and specialized blood tests can help diagnose these conditions.
Here’s an overview of neuromuscular junction disorders:
Myasthenia Gravis:

Myasthenia gravis is one of the most well-known NMJ disorders. It is an autoimmune disease in which the body’s immune system mistakenly targets and attacks receptors at the neuromuscular junction. This leads to muscle weakness, especially during periods of activity. Symptoms can include drooping eyelids, difficulty swallowing, and generalized muscle fatigue. Treatment often involves medications that improve neuromuscular transmission and, in some cases, immunosuppressive therapy.
Lambert-Eaton Myasthenic Syndrome (LEMS):
LEMS is a rare autoimmune disorder that affects the neuromuscular junction. It results in a reduction in the release of acetylcholine (a neurotransmitter) at the neuromuscular junction, leading to muscle weakness. LEMS is often associated with underlying malignancies, and treatment may involve addressing the underlying cancer, as well as medications to improve neuromuscular function.
Congenital Myasthenic Syndromes (CMS):
CMS are a group of genetic disorders that typically manifest in childhood or early adulthood. They result from mutations in genes that encode proteins involved in neuromuscular transmission. Depending on the specific genetic mutation, individuals with CMS can experience muscle weakness, fatigue, and other neuromuscular symptoms. Treatment varies depending on the subtype of CMS but may include medications to enhance neuromuscular function.
Botulism:
Botulism is a rare but serious condition caused by the ingestion of a toxin produced by the bacterium Clostridium botulinum. This toxin interferes with the release of acetylcholine at the neuromuscular junction, leading to muscle paralysis and potentially life-threatening respiratory problems. Treatment involves antitoxin administration and supportive care.
Drugs and Toxins:
Some drugs and toxins can interfere with neuromuscular transmission, leading to symptoms similar to NMJ disorders. For example, certain medications used in anesthesia or as muscle relaxants can affect the neuromuscular junction. These effects are usually reversible once the medication or toxin is eliminated from the body.
Diagnosis of NMJ disorders often involves specialized tests such as electromyography (EMG), nerve conduction studies, blood tests for specific antibodies (in the case of myasthenia gravis), and sometimes muscle biopsies. Treatment strategies aim to improve neuromuscular transmission, manage symptoms, and, in some cases, address underlying autoimmune or genetic factors.
Overall, neuromuscular junction disorders can have a significant impact on a person’s muscle function, and early diagnosis and appropriate management are essential to mitigate the effects and improve quality of life.
Similarities and Differences
Now, let’s delve into the similarities and differences between myopathy and neuromuscular junction disorders:
Similarities:
- Muscle Weakness: Both myopathies and NMJ disorders can result in muscle weakness, making it challenging for individuals to perform everyday activities.
- Impact on Mobility: These conditions can hinder a person’s mobility, leading to difficulties in walking, climbing stairs, and other routine tasks.
- Diagnostic Challenges: Both types of disorders may require specialized tests for accurate diagnosis. Muscle biopsies, genetic testing, and electromyography (EMG) are commonly used diagnostic tools.
Differences:
Site of Origin:
The fundamental difference lies in where these disorders originate. Myopathies originate within the muscle tissue, while NMJ disorders involve dysfunction at the neuromuscular junction.
Causes:
Myopathies have a broader range of causes, including genetic mutations, autoimmune responses, and environmental factors. In contrast, NMJ disorders often stem from autoimmune processes or genetic mutations specific to the neuromuscular junction.
Fluctuating Symptoms:
NMJ disorders are known for their fluctuating symptoms, with muscle weakness improving after periods of rest. Myopathies typically exhibit more constant muscle weakness.
Treatment Approaches:
Treatment approaches differ as well. Myopathy management may involve physical therapy, medications, and lifestyle adjustments. NMJ disorders often respond to therapies that target the immune system or enhance neuromuscular transmission, such as immunosuppressive drugs or acetylcholinesterase inhibitors.
Conclusion
In summary, myopathy and neuromuscular junction disorders are distinct categories of muscle disorders, differing in their origins, causes, clinical presentations, and treatment strategies. Understanding these differences is crucial for healthcare professionals to accurately diagnose and manage these conditions. If you or a loved one experiences symptoms related to muscle weakness or dysfunction, it’s essential to consult a healthcare provider for a thorough evaluation and diagnosis, as early intervention can significantly impact the course of these disorders and improve quality of life.

Dr. Kashouty, a diplomate of the American Board of Psychiatry and Neurology (ABPN), practices general neurology with fellowship trained specialization in clinical neurophysiology. Dr. Kashouty finds the form and function of the nerves and muscles the most interesting part of neurology, which is what led him to specialize in neurophysiology with more emphasis on neuromuscular conditions. He treats all neurological diseases, but his main focus is to treat and manage headaches, movement disorders and neuromuscular diseases.





