March is Multiple Sclerosis Awareness Month. Multiple Sclerosis (MS) is a complex and often unpredictable disease of the central nervous system that disrupts the flow of information within the brain, and between the brain and body. It presents a wide range of symptoms, which can vary greatly from person to person, making the journey to a definitive diagnosis and effective treatment plan a challenging one. In this blog post, we’ll explore the diagnostic process for MS, as well as the current treatment options available to those living with this condition.
The Diagnostic Maze: Identifying MS
The process of diagnosing Multiple Sclerosis (MS) is as complex as the disease itself, requiring a careful and methodical approach by neurologists to ensure accuracy. Given that MS symptoms can mimic those of many other neurological conditions, neurologists employ a multifaceted strategy to rule out other causes and confirm the presence of MS. Here’s a closer look at the diagnostic process:
1. Initial Assessment
The journey often begins with the patient’s medical history and a detailed account of symptoms, including their onset, duration, and pattern. Neurologists pay close attention to the type of symptoms, their progression, and any relapses or remissions. This historical insight is crucial, as MS is characterized by symptoms that can fluctuate and recur over time.
2. Neurological Examination
A comprehensive neurological examination follows, where the neurologist assesses functions such as vision, balance, coordination, strength, and reflexes. This exam helps identify impairments that may be indicative of central nervous system involvement, a hallmark of MS.
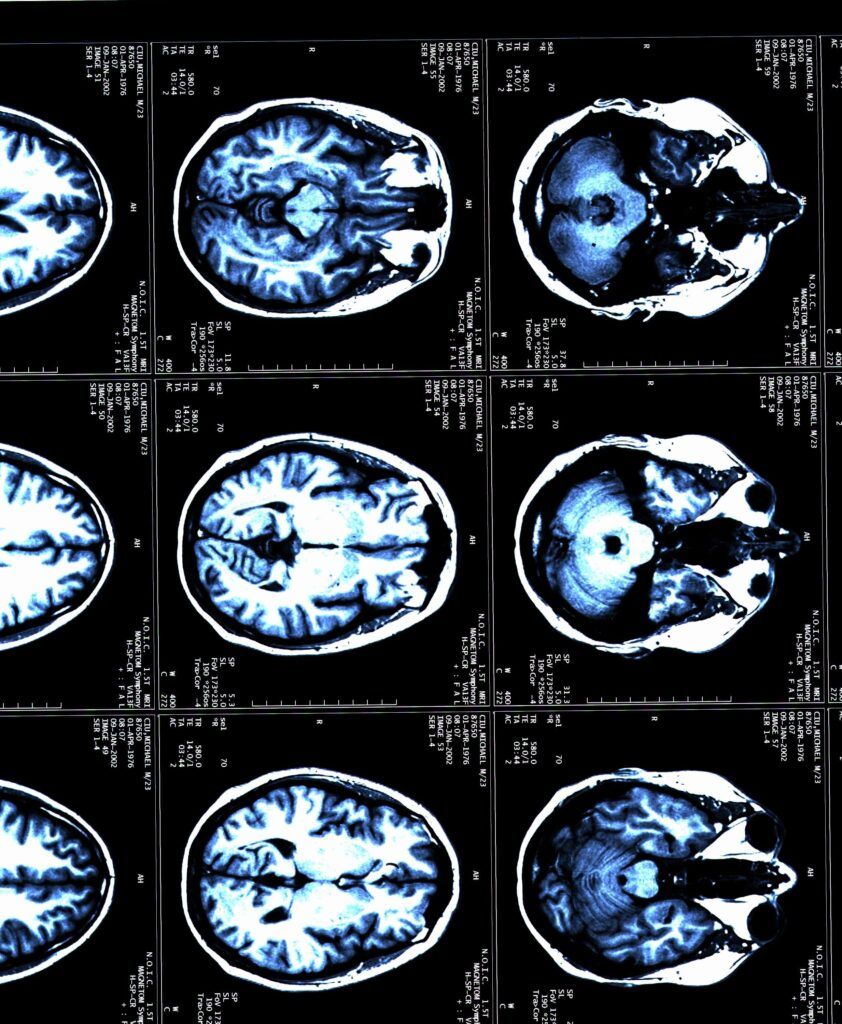
3. Magnetic Resonance Imaging (MRI)
MRI scans are pivotal in the MS diagnostic process. They provide detailed images of the brain and spinal cord, revealing lesions or areas of demyelination that suggest MS. Neurologists often use MRI scans to look for evidence of damage in multiple areas of the central nervous system that occurred at different times. The use of contrast material (gadolinium) can help distinguish between old and new lesions, offering insights into the disease’s activity.
4. Lumbar Puncture (Spinal Tap)
Though not always required, a lumbar puncture may be performed to analyze cerebrospinal fluid (CSF) – the fluid surrounding the brain and spinal cord. This test looks for abnormalities linked to MS, such as elevated levels of specific proteins or the presence of oligoclonal bands, which are bands of immunoglobulins found in the CSF of most people with MS.
5. Evoked Potential Tests
Evoked potential tests measure the electrical activity in the brain in response to visual, auditory, or sensory stimuli. These tests can detect slowed responses due to MS-related nerve damage, even when symptoms are not present, providing additional evidence of MS.
6. Ruling Out Other Conditions
An essential part of diagnosing MS is the exclusion of other conditions that could cause similar symptoms. Conditions like Lyme disease, vitamin B12 deficiency, and lupus (among others) can mimic MS, so neurologists often perform a variety of tests to rule these out. This process ensures that the diagnosis of MS is made with a high degree of confidence.
The McDonald Criteria: A Diagnostic Tool for MS
The McDonald Criteria is a tool that neurologists use to facilitate the diagnosis of MS. Updated periodically to reflect advances in understanding and technology, these criteria incorporate the findings from MRI scans, clinical assessments, and additional tests like CSF analysis. The McDonald Criteria allow for an earlier and more accurate diagnosis of MS by defining specific guidelines regarding the evidence of damage in the central nervous system and its dissemination in time and space.
Emphasizing Early and Accurate Diagnosis
Early and accurate diagnosis is crucial in managing MS effectively. It enables timely initiation of treatment to manage symptoms, reduce relapses, and potentially slow disease progression. The diagnostic process for MS reflects the complexity of the disease but is designed to ensure that patients receive a precise diagnosis and the best possible care.
Embarking on Treatment: Options and Strategies
Treatment options for Multiple Sclerosis (MS) are multifaceted and tailored to manage the disease’s complex nature, aiming to reduce disease activity, manage symptoms, and improve quality of life. The landscape of MS treatment has evolved significantly, offering patients a variety of therapeutic approaches. Here’s an overview of the available treatment options:
1. Disease-Modifying Therapies (DMTs)
DMTs are at the forefront of MS treatment, designed to reduce the frequency and severity of relapses, slow the progression of disability, and limit new disease activity as seen on MRI scans. These medications target the disease’s inflammatory processes and can be categorized based on their mode of administration:
- Injectables: Include interferon beta preparations and glatiramer acetate, which have been used for many years and are often considered for initial therapy.
- Oral Medications: Such as fingolimod, dimethyl fumarate, teriflunomide, and siponimod, offer an alternative to injections and vary in mechanism of action and side effect profiles.
- Infusions: High-efficacy treatments like natalizumab, ocrelizumab, alemtuzumab, and rituximab are administered through intravenous infusion and are typically used for more aggressive forms of MS or when other therapies have failed.
2. Treatment for MS Relapses
Relapses or exacerbations of MS, characterized by new or worsening neurological symptoms, are often treated with corticosteroids to reduce inflammation. Intravenous methylprednisolone is the most common treatment, sometimes followed by a tapering course of oral steroids. For severe relapses not responding to steroids, plasmapheresis (plasma exchange) might be considered.
3. Symptomatic Treatments

Symptomatic treatments in MS are crucial for improving the quality of life and are tailored to the specific symptoms each patient experiences. These can include:
- Mobility and Spasticity: Physical therapy, muscle relaxants (e.g., baclofen, tizanidine), and sometimes botulinum toxin injections.
- Fatigue: Management strategies include energy conservation techniques, exercise, and medications like amantadine or modafinil.
- Pain: Neuropathic pain treatments include anticonvulsants (e.g., gabapentin, pregabalin) and antidepressants (e.g., amitriptyline, duloxetine).
- Bladder and Bowel Issues: Anticholinergics for bladder control and dietary modifications, laxatives, or stool softeners for bowel management.
- Cognitive and Emotional Health: Cognitive rehabilitation and psychotherapy, along with medications for mood disorders.
4. Lifestyle Modifications and Complementary Therapies
Lifestyle changes and complementary therapies can play an important role in managing MS:
- Diet and Nutrition: While no specific diet has been proven to alter the course of MS, healthy eating patterns can support overall well-being.
- Exercise: Regular physical activity can help improve strength, fatigue, mobility, and mood.
- Stress Management: Techniques such as meditation, yoga, and mindfulness can help manage stress, which may exacerbate symptoms.
- Alternative Therapies: Some patients find relief with acupuncture, massage, or other complementary therapies, although these should not replace conventional treatments.
5. Medical Cannabis
The use of medical marijuana for treating symptoms of Multiple Sclerosis (MS) has garnered significant interest and research in recent years.
- Active compounds in cannabis, such as THC (tetrahydrocannabinol) and CBD (cannabidiol), have been explored for their potential to alleviate various MS symptoms, including pain, muscle stiffness (spasticity), and sleep disturbances.
- Clinical studies suggest that medical marijuana may provide relief for some individuals with MS, leading to improvements in quality of life and functional outcomes.
- Healthcare professionals recommend careful consideration of the benefits versus potential side effects, such as cognitive impairment, dizziness, and interactions with other medications.
6. Emerging Therapies
The field of MS research is active, with ongoing clinical trials investigating new treatments, including stem cell transplantation and therapies targeting specific immune mechanisms. These emerging therapies offer hope for even more effective treatments in the future.
Tailored Treatment Plans
It’s important to note that MS treatment is highly individualized. Neurologists work closely with patients to develop a treatment plan that suits their specific form of the disease, lifestyle, and treatment goals. Regular monitoring through clinical evaluations and MRI scans is crucial to assess the effectiveness of treatment and make adjustments as needed.
Conclusion
In conclusion, navigating the complexities of Multiple Sclerosis (MS) requires a comprehensive and personalized approach to diagnosis and treatment. From the intricate process of diagnosing the condition through a combination of clinical evaluations, MRI scans, and other diagnostic tools, to the wide array of treatment options including disease-modifying therapies, symptomatic treatments, and lifestyle modifications, managing MS is a multifaceted endeavor. The potential role of medical marijuana in symptom management further highlights the evolving landscape of MS treatment options, underscoring the importance of ongoing research and individualized care plans. As our understanding of MS deepens and treatment strategies continue to advance, there is renewed hope for individuals living with MS to lead fulfilling lives with improved quality of life and potentially slower disease progression.

Dr. Kashouty, a diplomate of the American Board of Psychiatry and Neurology (ABPN), practices general neurology with fellowship trained specialization in clinical neurophysiology. Dr. Kashouty finds the form and function of the nerves and muscles the most interesting part of neurology, which is what led him to specialize in neurophysiology with more emphasis on neuromuscular conditions. He treats all neurological diseases, but his main focus is to treat and manage headaches, movement disorders and neuromuscular diseases.