The fascinating intersection of neurology and systemic health is an area where the complexity of the human body reveals itself in profound ways. Systemic diseases, those that impact multiple organs or the entire body, can have a significant and sometimes surprising influence on the nervous system. These influences manifest through a spectrum of neurological symptoms that can be both revealing and challenging to interpret. In this blog, we will delve into how diseases that primarily affect other parts of the body can lead to neurological complications, the importance of early recognition of these symptoms, and the latest advancements in treatment and management. Our journey through this topic will not only highlight the interconnected nature of our body systems but also underscore the importance of a holistic approach to healthcare and disease management.
Understanding the Connection
The connection between systemic diseases and neurological manifestations is a compelling example of the intricate interplay within the human body. Systemic diseases, which affect multiple organs or the entire system, can have profound and often unexpected effects on the nervous system. This relationship is governed by a complex web of physiological processes, including immune responses, metabolic changes, and vascular alterations. For instance, conditions like diabetes mellitus can lead to neuropathies due to prolonged high blood sugar damaging nerve fibers. Similarly, autoimmune diseases such as lupus can trigger inflammatory processes that affect the brain and spinal cord, leading to a range of neurological symptoms. In other cases, like with certain cancers, the body’s immune response to systemic illness can inadvertently impact neurological function, resulting in conditions such as paraneoplastic neurological disorders. Understanding this connection is vital, as it not only aids in the early detection and treatment of neurological complications arising from systemic diseases but also underscores the need for a holistic approach in healthcare, recognizing the body as an interconnected system rather than a collection of isolated parts.
Common Systemic Diseases with Neurological Manifestations
Diabetes Mellitus:
Diabetes, a prevalent systemic disease characterized by high blood sugar levels, can manifest neurologically in various significant ways, primarily through diabetic neuropathy. This condition is a direct consequence of prolonged hyperglycemia, which damages the small blood vessels that supply nerves, leading to nerve dysfunction. Patients often experience symptoms like numbness, tingling, and pain, predominantly in the extremities, known as peripheral neuropathy. Diabetic neuropathy can also affect autonomic functions, leading to issues such as gastrointestinal disturbances, cardiovascular irregularities, and urinary problems. In some cases, diabetes can lead to more acute neurological manifestations like diabetic amyotrophy, causing severe pain and muscle weakness, primarily in the thigh muscles. Moreover, diabetes increases the risk of stroke and other cerebrovascular diseases due to its impact on blood vessels. These neurological manifestations of diabetes highlight the importance of stringent blood sugar control and comprehensive management to prevent or mitigate these complications.
Lupus:
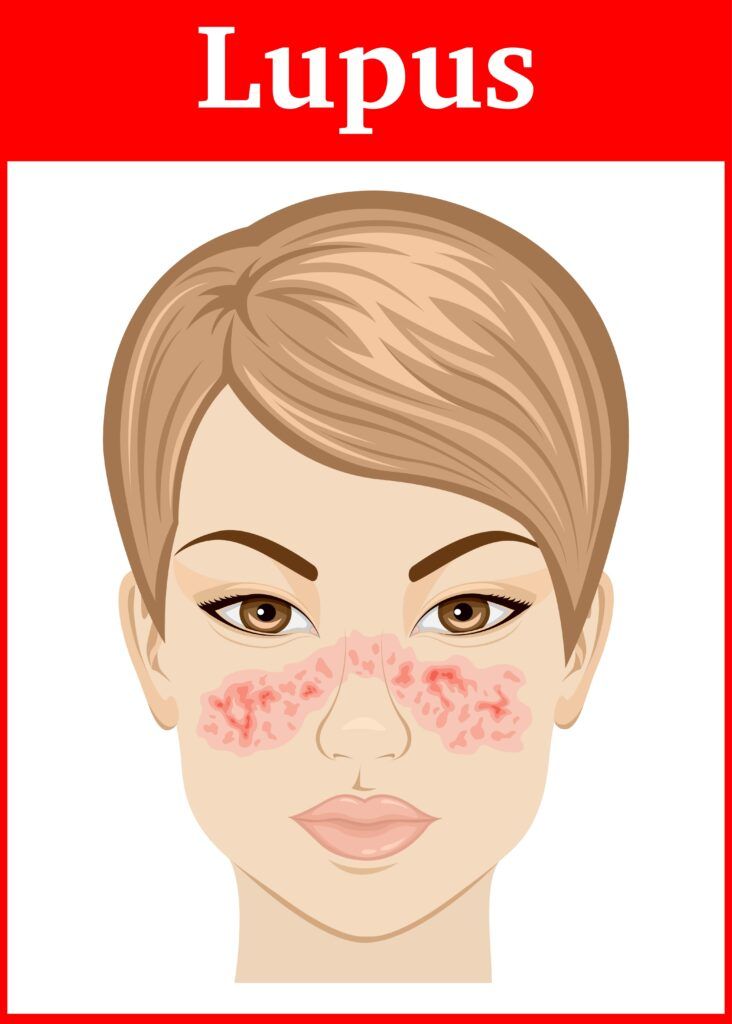
Lupus, a chronic autoimmune disease, can manifest neurologically in a variety of ways, a condition often referred to as neuropsychiatric systemic lupus erythematosus (NPSLE). The immune system in lupus patients mistakenly attacks healthy tissue, including that of the nervous system, leading to inflammation and a wide range of neurological and psychiatric symptoms. These manifestations can be diverse, ranging from mild to severe. Patients may experience headaches, which can be frequent and severe, and in some cases, mimic migraines. Cognitive dysfunctions, including confusion, difficulty concentrating, and memory problems, are also common. More severe neurological complications include seizures and stroke, resulting from inflammation in the brain and nervous system. Additionally, lupus can cause mood disorders like depression and anxiety. Peripheral neuropathy, presenting as numbness, tingling, or pain in the limbs, can also occur. The varied neurological manifestations of lupus underscore the importance of early recognition and treatment to manage these symptoms effectively and improve the overall quality of life for those affected.
Rheumatoid Arthritis:
Rheumatoid arthritis (RA), predominantly known as a chronic inflammatory disorder affecting the joints, can also manifest neurologically in several ways. One of the most common neurological complications is peripheral neuropathy, where patients experience numbness, tingling, and pain, typically in their hands and feet, due to nerve inflammation or compression. Cervical myelopathy is another serious condition that can occur in RA patients, particularly when the disease affects the cervical spine. This can lead to compression of the spinal cord, resulting in symptoms like neck pain, weakness in the arms and legs, and in severe cases, difficulties with coordination and bladder control. Rheumatoid arthritis can also lead to the development of carpal tunnel syndrome, a condition caused by compression of the median nerve in the wrist, leading to pain and numbness in the hand. Additionally, RA’s systemic nature means it can contribute to vasculitis, an inflammation of the blood vessels, which can affect brain function and potentially lead to stroke-like symptoms. The neurological manifestations of rheumatoid arthritis highlight the need for comprehensive care and monitoring of RA patients, not only for their joint health but also for potential neurological complications.
HIV/AIDS:
HIV/AIDS, a disease known primarily for its profound impact on the immune system, can also manifest neurologically, a condition referred to as HIV-associated neurocognitive disorders (HAND). As the virus compromises the immune system, it can directly invade and damage the nervous system, including the brain, spinal cord, and peripheral nerves. This invasion can lead to a spectrum of neurological symptoms, ranging from mild cognitive impairments, such as memory loss and difficulty concentrating, to more severe conditions like HIV-associated dementia. Patients may also experience peripheral neuropathy, characterized by numbness, tingling, and pain in the extremities, as well as motor symptoms like weakness and loss of coordination. In advanced stages, HIV/AIDS can cause more serious complications like encephalitis, an inflammation of the brain, leading to severe neurological deficits. Additionally, as the immune system weakens, patients become more susceptible to opportunistic infections and cancers that can further affect the nervous system. The neurological manifestations of HIV/AIDS underscore the importance of early diagnosis and antiretroviral therapy, not only to manage the systemic impact of the disease but also to mitigate its neurological effects.
Cancer:
Cancer can manifest neurologically in several complex ways, primarily when cancer cells spread to the nervous system or when the body’s immune response to cancer affects neurological function. Metastatic spread to the brain or spinal cord can lead to symptoms such as headaches, seizures, sensory changes, and motor dysfunction, depending on the location and size of the metastases. Another significant neurological impact of cancer is the development of paraneoplastic syndromes, where the immune system’s response to a tumor elsewhere in the body inadvertently damages nervous system tissues. These syndromes can manifest as a wide array of symptoms, including cognitive impairments, limb weakness, sensory disturbances, and movement disorders. Additionally, certain cancers, particularly those involving the blood or lymphatic system, can lead to conditions like peripheral neuropathy, causing pain, numbness, and weakness in the limbs. Treatments for cancer, such as chemotherapy and radiation, can also contribute to neurological complications, sometimes leading to cognitive dysfunction, known as “chemo brain,” or peripheral nerve damage. The neurological manifestations of cancer highlight the need for a multidisciplinary approach in cancer treatment, one that addresses not only the oncological aspects but also the potential neurological impacts to improve patient care and quality of life.
Diagnostic Challenges and Neurological Assessment in Systemic Diseases
Diagnosing neurological manifestations associated with systemic diseases presents unique challenges, often requiring a meticulous and comprehensive approach by neurologists and other specialists. The complexity arises from the overlapping symptoms between primary neurological disorders and those secondary to systemic diseases, such as diabetes, lupus, or HIV/AIDS.
Understanding the Challenges
- Non-Specific Symptoms: Neurological symptoms like numbness, cognitive impairment, or fatigue are non-specific and can be seen in a myriad of conditions, making the diagnostic process challenging.
- Diverse Manifestations: Systemic diseases can affect the nervous system in various ways, leading to a wide range of symptoms, from peripheral neuropathy to severe cognitive decline.
- Complex Interactions: The interaction between systemic disease processes and the nervous system is complex, often leading to symptoms that can be misleading or difficult to interpret.
Neurological Assessment Strategies
To navigate these challenges, neurologists employ a structured approach to diagnose these conditions accurately:
- Detailed Medical History: A thorough medical history is crucial. Neurologists probe for the duration, progression, and specific characteristics of symptoms. They also look for a history of systemic diseases like diabetes or rheumatoid arthritis, which could point towards a secondary neurological condition.
- Physical and Neurological Examination: A comprehensive physical examination, including a detailed neurological assessment, is performed. This involves evaluating muscle strength, reflexes, coordination, sensation, and cognitive functions.
- Diagnostic Testing:

- Blood Tests: These are used to detect markers of systemic diseases, such as elevated blood sugar levels in diabetes or autoimmune markers in lupus.
- Imaging Studies: MRI or CT scans are critical in assessing structural changes in the brain and spinal cord that could be related to systemic diseases.
- Nerve Conduction Studies and Electromyography (EMG): These tests are particularly useful in diagnosing conditions like peripheral neuropathy.
- Lumbar Puncture: Sometimes necessary to analyze cerebrospinal fluid, especially in cases where infections or autoimmune conditions are suspected.
- Multidisciplinary Collaboration: Given the complexity, neurologists often collaborate with other specialists, such as rheumatologists, endocrinologists, and oncologists, to integrate findings and develop a comprehensive understanding of the patient’s condition.
- Monitoring and Reevaluation: Neurological symptoms related to systemic diseases may evolve over time. Continuous monitoring and periodic reevaluation are essential components of the diagnostic process.
Conclusion
The neurological manifestations of systemic diseases are a vital aspect of understanding the overall impact of these conditions on the human body. Early recognition and appropriate management can significantly improve patient outcomes. Neurologists play a pivotal role in unraveling the complex relationship between these conditions, employing a variety of diagnostic tools and collaborating with other healthcare professionals to ensure accurate diagnosis and effective management. This holistic approach is fundamental in addressing the multifaceted nature of these conditions, ultimately leading to better patient outcomes.

Dr. Kashouty, a diplomate of the American Board of Psychiatry and Neurology (ABPN), practices general neurology with fellowship trained specialization in clinical neurophysiology. Dr. Kashouty finds the form and function of the nerves and muscles the most interesting part of neurology, which is what led him to specialize in neurophysiology with more emphasis on neuromuscular conditions. He treats all neurological diseases, but his main focus is to treat and manage headaches, movement disorders and neuromuscular diseases.




