Peripheral neuropathy, a common neurological disorder, affects millions of people worldwide. It occurs when nerves outside the brain and spinal cord—known as peripheral nerves—are damaged, leading to a variety of symptoms that can significantly impact daily life. This condition manifests in numerous forms, including sensory, motor, and autonomic neuropathy, each affecting different nerve functions. The causes of peripheral neuropathy are diverse, ranging from diabetes and autoimmune diseases to genetic factors and environmental exposures. Understanding the nature of this disorder, its diagnostic processes, and the effective management strategies available is essential for those affected. This blog aims to delve into the intricacies of peripheral neuropathy, offering insight into its causes and discussing comprehensive management strategies to alleviate symptoms and improve quality of life.
In This Blog:
- Understanding Peripheral Neuropathy
- Causes of Peripheral Neuropathy
- Diagnosing Peripheral Neuropathy
- Management Strategies for Peripheral Neuropathy
Understanding Peripheral Neuropathy
Peripheral neuropathy refers to a condition where the peripheral nerves, which transmit information between the brain and spinal cord and the rest of the body, become damaged or dysfunctional. This nerve damage can manifest in various ways, depending on which nerves are affected. The most commonly recognized categories of peripheral neuropathy include:
Sensory Neuropathy:
This type affects the nerves responsible for sensation. Patients may experience pain, tingling, numbness, or a loss of sensation, primarily in the hands and feet. Sensory neuropathy can be particularly distressing as it may lead to injuries going unnoticed, which can result in complications.
Motor Neuropathy:
This type impacts the nerves that control muscle movement. Symptoms might include muscle weakness, cramps, and spasms. Severe motor neuropathy can lead to muscle wasting and decreased mobility.
Autonomic Neuropathy:
This form affects the nerves that control involuntary bodily functions such as heart rate, blood pressure, digestion, and bladder function. Symptoms can be wide-ranging, from digestive issues to changes in sweating patterns and difficulties in regulating blood pressure.
Each type of peripheral neuropathy can significantly impair a person’s quality of life by interfering with daily activities and personal independence. The symptoms themselves are highly variable and can develop suddenly or gradually. They may also fluctuate in intensity or be persistent. For some, the symptoms might be mild, while for others, they can be debilitating and even incapacitating.
Understanding these symptoms is crucial for early detection and management of the condition. The diverse manifestations of peripheral neuropathy underline the importance of a comprehensive diagnostic approach to tailor an effective treatment plan for each individual, addressing their specific type of nerve damage and related symptoms.
Causes of Peripheral Neuropathy
Peripheral neuropathy can stem from a variety of causes, each contributing to nerve damage in distinct ways. Understanding these causes is crucial for both diagnosis and the development of targeted treatments. Here are some of the most common causes of peripheral neuropathy:
Diabetes:
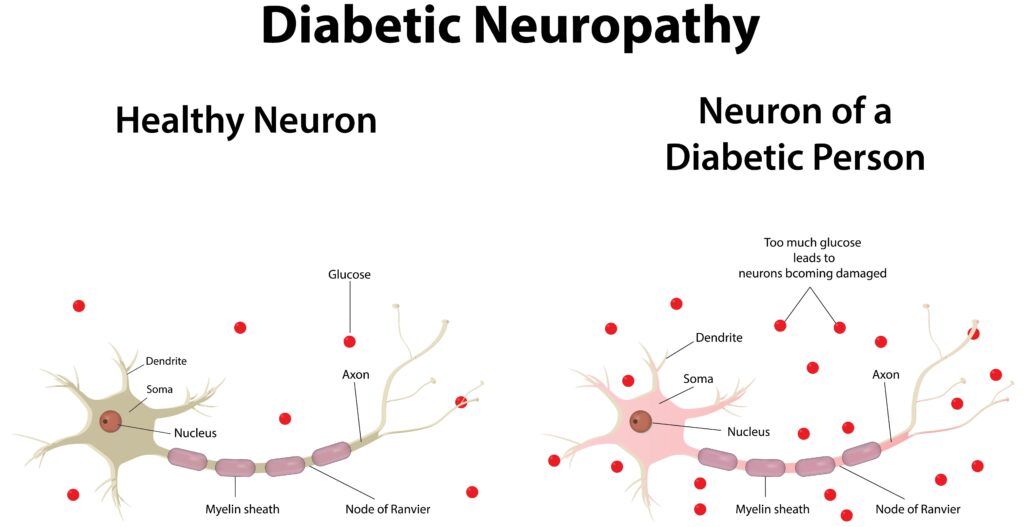
This is the leading cause of peripheral neuropathy. High blood sugar levels associated with diabetes can damage nerves over time, particularly in the legs and feet. This type of neuropathy is known as diabetic neuropathy and affects up to 50% of people with diabetes.
Autoimmune Diseases:
Conditions like rheumatoid arthritis, lupus, and Sjögren’s syndrome can lead to inflammatory processes that affect nerves. Guillain-Barré syndrome, although rare, is another autoimmune condition that can cause acute, severe peripheral nerve damage.
Infections:
Some viral and bacterial infections can directly attack nerve tissues or cause nerve damage as a secondary effect of inflammation. For example, Lyme disease, shingles (varicella-zoster virus), and HIV are known to be associated with peripheral neuropathy.
Hereditary Disorders:
Certain genetic conditions, such as Charcot-Marie-Tooth disease, are inherited forms of neuropathy. These disorders cause abnormal nerve structure or function from a young age, leading to progressive nerve damage.
Exposure to Toxins:
Chemicals and heavy metals like lead, arsenic, mercury, and organic solvents can cause toxic neuropathy. Additionally, excessive alcohol consumption can lead to nutrient deficiencies that harm peripheral nerves.
Nutritional Deficiencies:
Deficiencies in B vitamins, particularly B12, B6, and folate, are critical for nerve health and function. Lack of these nutrients can lead to significant nerve damage.
Lifestyle factors also play a significant role in the risk of developing peripheral neuropathy. For instance, poor dietary choices, alcohol abuse, and exposure to toxins through occupation or environment can all contribute to nerve damage. Recognizing these factors is vital for prevention and early intervention, which can mitigate the severity of peripheral neuropathy and improve outcomes.
Diagnosing Peripheral Neuropathy
Accurate diagnosis of peripheral neuropathy is essential for effective management and treatment. The diagnostic process typically begins with a comprehensive medical history review and physical examination, followed by a series of specific tests to identify the underlying causes and assess the extent of nerve damage. Here’s how healthcare providers approach the diagnosis of this condition:
Physical and Neurological Examinations:
Initially, doctors conduct thorough physical exams that may include checking tendon reflexes, muscle strength, and tone, as well as the ability to feel certain sensations. A neurological exam helps pinpoint the areas affected and the type of nerve fibers involved.
Blood Tests:
These can reveal diabetes, vitamin deficiencies, liver or kidney dysfunction, and other metabolic disorders that might cause neuropathy. Blood tests can also detect markers of autoimmune diseases and infections that could be linked to neuropathy.
Electromyography (EMG) and Nerve Conduction Studies:

EMG measures the electrical activity of muscles and helps determine if muscle weakness is due to muscle injury or nerve damage. Nerve conduction studies, on the other hand, measure how quickly and effectively nerves can send electrical signals. These tests are crucial for distinguishing between different types of neuropathy and identifying the specific nerves involved.
Additional Tests:
Depending on the suspected cause, additional tests may be performed. These could include:
- Skin biopsies to evaluate the number and condition of nerve endings,
- Nerve biopsy to look at a small sample of a nerve under the microscope,
- Imaging tests, such as MRI or CT scans, to rule out other causes of symptoms like tumors or herniated discs.
Early diagnosis is crucial in managing peripheral neuropathy effectively. By pinpointing the type and extent of nerve damage, healthcare providers can tailor treatment plans that address both the underlying cause and the symptoms, thereby improving the patient’s quality of life and preventing further complications.
Management Strategies for Peripheral Neuropathy
Managing peripheral neuropathy involves addressing the underlying cause of the nerve damage as well as alleviating the symptoms to improve the quality of life. Here is a detailed look at the treatment options available:
Medications:
- Pain Relievers: Over-the-counter pain medications may be used for mild symptoms. For more severe pain, prescription-strength pain relievers might be necessary.
- Anti-seizure Medications: Drugs originally designed to treat epilepsy may help relieve nerve pain. These include gabapentin and pregabalin, which can reduce the painful symptoms of neuropathy.
- Antidepressants: Certain antidepressants, such as tricyclic antidepressants and serotonin-norepinephrine reuptake inhibitors (SNRIs), can help ease pain by altering chemical processes in the brain that cause you to feel pain.
Non-Pharmacological Therapies:

- Physical Therapy: This can help improve mobility and prevent muscle wasting in patients with motor neuropathy. Physical therapists may also teach exercises that can help maintain muscle strength and reduce cramps and pain.
- Occupational Therapy: For those struggling with daily tasks due to their symptoms, occupational therapy can offer strategies to cope with numbness and loss of fine motor skills, making everyday activities easier.
- Lifestyle Modifications: Diet and exercise are critical. Managing blood sugar levels, for example, can slow the progression of diabetic neuropathy. Nutritional counseling can also help correct deficiencies known to contribute to neuropathy.
Advanced Treatments and Research:
- Capsaicin Cream and Lidocaine Patches: Topical treatments like capsaicin cream can reduce pain sensations, while lidocaine patches provide temporary numbness to ease nerve pain.
- Electrical Nerve Stimulation: Techniques such as transcutaneous electrical nerve stimulation (TENS) can reduce neuropathic pain for some people by delivering a variable electrical current to nerve pathways.
- Experimental Approaches: Ongoing research into gene therapy and stem cells holds promise for repairing or regenerating damaged nerves, though these treatments are still largely in the experimental stages.
- Medical Cannabis: Some studies suggest that medical cannabis may be effective in managing pain associated with peripheral neuropathy. Cannabinoids, the active components of cannabis, are believed to reduce pain through their interaction with the body’s endocannabinoid system.
Effective management of peripheral neuropathy requires a comprehensive approach that combines medical treatment with physical and lifestyle interventions. Regular follow-ups with healthcare providers are important to adjust treatment strategies based on the progression of the disease and the response to treatment. This personalized care approach helps patients maintain their independence and improve their overall quality of life despite their condition.
Conclusion
Peripheral neuropathy presents a complex challenge due to its diverse causes and manifestations, but understanding its underlying mechanisms and symptoms is the first step toward effective management. By exploring a combination of medical treatments, physical therapies, and lifestyle adjustments, individuals suffering from this condition can find significant relief and maintain a high quality of life. It is crucial for those experiencing symptoms to seek timely medical advice to tailor a treatment plan that addresses their specific needs. With ongoing research and advancements in treatment options, there is hope for even better management strategies in the future, potentially offering greater relief for those affected by this debilitating condition.

Dr. Kashouty, a diplomate of the American Board of Psychiatry and Neurology (ABPN), practices general neurology with fellowship trained specialization in clinical neurophysiology. Dr. Kashouty finds the form and function of the nerves and muscles the most interesting part of neurology, which is what led him to specialize in neurophysiology with more emphasis on neuromuscular conditions. He treats all neurological diseases, but his main focus is to treat and manage headaches, movement disorders and neuromuscular diseases.




