Pain, a universally experienced phenomenon, serves as a crucial biological signal alerting us to potential harm and requiring attention. Yet, the way our brains interpret this signal—transforming raw sensory input into the subjective experience of pain—is a complex process, influenced by both physiological and psychological factors. In this blog post, we’ll explore the intricate neurology of pain, from the initial detection by nociceptors to the intricate processing within the brain. Additionally, as attitudes toward pain management evolve, we’ll delve into the role of medical cannabis, a treatment option that has gained traction and legitimacy in the medical community for its efficacy in managing various types of pain. This exploration aims to shed light on the multifaceted nature of pain and the modern approaches to its management, offering insights into how these methods can enhance quality of life for those afflicted.
In This Blog:
- Understanding Pain
- The Brain’s Role in Pain Perception
- Psychological Aspects of Pain
- Medical Cannabis and Pain Management
Understanding Pain
Pain is a vital communication tool for the body, signaling when something is amiss and potentially harmful. It can be broadly categorized into two types: acute and chronic. Acute pain serves as an immediate response to injury, alerting us to potential damage and often resolving as the body heals. Conversely, chronic pain persists beyond the expected period of healing, becoming a disease in its own right due to its long duration and the complex body responses it invokes.
The Biological Purpose of Pain
The primary biological purpose of pain is protective. It encourages behaviors that prevent further bodily harm and promotes healing. For example, the pain associated with touching a hot stove teaches us to withdraw our hand quickly, preventing burns. This kind of pain, though unpleasant, is essential for survival by helping individuals avoid dangerous situations and prompting care for injuries.
Pain Pathway: From Nociceptors to the Brain
Pain perception begins at the point of injury where specialized nerve cells, known as nociceptors, detect damage. These receptors are capable of responding to various stimuli such as extreme heat, cold, or pressure, and chemical signals released from damaged cells. Once activated, nociceptors transmit signals through sensory neurons to the spinal cord and up to the brain.
- Transduction: At the site of injury, the nociceptors convert the damaging stimuli into electrical signals.
- Transmission: These electrical signals are then sent through nerve fibers to the spinal cord and onto the brain.
- Modulation: As signals pass through the spinal cord, they can be either amplified or dampened before reaching the brain, influenced by various neurotransmitters and modulators.
- Perception: When the pain signals reach the brain, they are processed and interpreted in several regions, including the thalamus, cortex, and limbic system. This is where pain becomes a conscious, subjective experience.
The entire pathway, from detection to perception, is not just a straightforward relay of information. It is a dynamic interplay between different types of neurons and pathways, with the brain having the capability to modulate the intensity and emotional response to pain. This sophisticated processing ensures that pain is not merely a signal, but a complex experience shaped by both the body and mind, which can be influenced by a person’s emotional state, previous experiences, and cultural context. Understanding this pathway is crucial for developing effective pain management strategies, highlighting the need for approaches that address both the physical and psychological aspects of pain.
The Brain’s Role in Pain Perception
Pain perception is not merely a signal that travels unimpeded from the point of injury to the brain; rather, it involves complex processing by various brain regions that interpret and modulate the pain experience. Understanding how the brain processes pain signals is crucial for both diagnosing and treating pain disorders.
How Pain Signals Are Processed in the Brain
Once pain signals reach the brain via the spinal cord, they are distributed to several key areas for further processing:
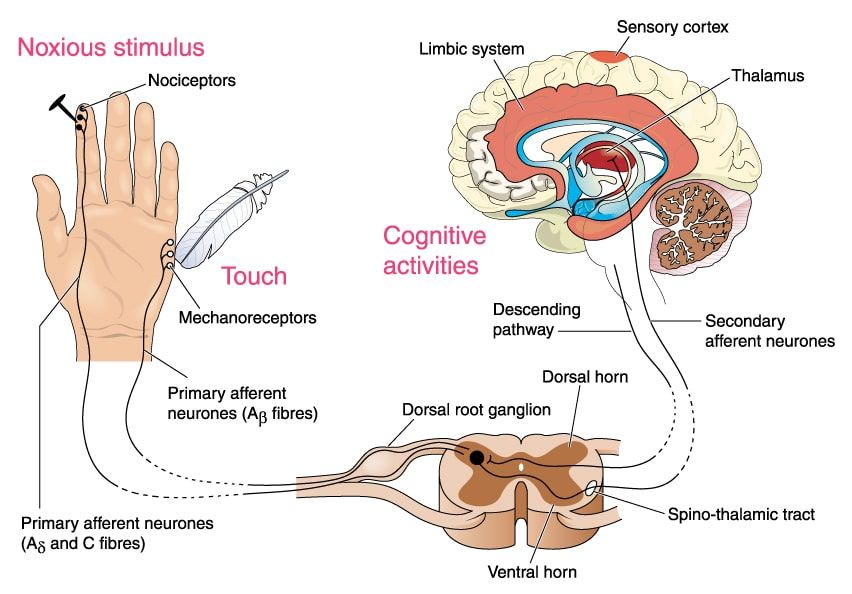
- The Thalamus acts as the brain’s relay station, where almost all sensory information, including pain, is first sent to be forwarded to other specific brain areas.
- The Cerebral Cortex is responsible for thinking and processing information from the senses. Different parts of the cortex contribute to interpreting the intensity and location of pain, as well as comparing it to past experiences and contextual information.
- The Limbic System, particularly areas like the amygdala and hippocampus, processes the emotional aspects of pain. This area can amplify the perception of pain if the emotional response is strong, linking pain to mood and anxiety levels.
Regions of the Brain Involved in Pain Perception
In addition to the thalamus, cortex, and limbic system, several other regions play critical roles:
- The Frontal Cortex is involved in the cognitive aspects of pain, such as attention and expectation, which can significantly affect the perception of pain intensity.
- The Insula has a role in empathizing with and internalizing the pain, integrating pain with autonomic responses in the body, and has been implicated in chronic pain conditions.
- The Brainstem regulates the flow of messages between the brain and the body and can activate descending pathways that modulate pain, providing an internal mechanism for pain relief.
Neuroplasticity and Pain
Chronic pain can lead to changes in the brain’s structure and function, a phenomenon known as neuroplasticity. These changes can include alterations in the brain’s electrical activity, increases in certain areas’ size that process pain signals, and decreases in others that might mitigate pain. This plasticity not only affects how pain is perceived but can also contribute to the persistence of pain even after the original injuries have healed. It suggests that pain, especially chronic pain, is more than a simple response to physical injury; it can evolve into a complex, self-perpetuating cycle that involves multiple brain regions and processes.
Understanding the brain’s role in pain perception highlights the complexity of pain as a sensory and emotional experience. It also underscores the importance of addressing psychological and neurological factors in pain management, pointing towards treatments that encompass both physical and mental health interventions.
Psychological Aspects of Pain
Pain is not only a physical sensation but also profoundly influenced by psychological factors. The subjective nature of pain means that individual experiences can vary widely, even under similar physical circumstances. This section explores how psychological aspects affect pain perception and the interplay between mental health and physical pain.
Influence of Psychological Factors on Pain Perception
The experience of pain can be significantly shaped by psychological conditions, including stress, anxiety, and depression. These conditions can enhance the brain’s sensitivity to pain by altering how pain signals are processed:
- Stress increases the body’s levels of cortisol and adrenaline, which can heighten sensitivity to pain by increasing inflammation and affecting the nervous system’s normal functioning.
- Anxiety often leads to a hyperawareness of bodily sensations, which can amplify perceptions of pain and create a vicious cycle of pain and anxiety.
- Depression can lower the body’s natural pain threshold, making individuals more susceptible to chronic pain conditions.
Pain Threshold and Pain Tolerance
- Pain threshold refers to the point at which a stimulus begins to be perceived as painful. This threshold varies widely among individuals and can be influenced by psychological factors, such as one’s emotional state or distractions.
- Pain tolerance is the maximum level of pain a person can handle before it becomes unbearable. Pain tolerance is also subjective and can be increased or decreased by psychological factors like mood, beliefs, and prior experiences with pain.
Role of Emotions, Stress, and Mental Health
The relationship between pain and emotions is bidirectional:
- Emotional responses to pain can exacerbate the perception of pain, making it more difficult to manage and treat. For example, feelings of helplessness or hopelessness, often associated with chronic pain conditions, can worsen the emotional and physical experience of pain.
- Conversely, effective management of emotional responses can reduce the perception of pain. Techniques such as cognitive-behavioral therapy (CBT), mindfulness, and relaxation exercises have been shown to lower pain sensitivity by altering psychological responses to pain.
Understanding the psychological aspects of pain is crucial for developing comprehensive pain management strategies. It not only helps in addressing the physical symptoms but also the emotional and psychological challenges that accompany pain. Integrating psychological therapy into pain management protocols can provide patients with tools to better control their pain and improve their overall quality of life, suggesting a holistic approach to treating pain that addresses both mind and body.
Medical Cannabis and Pain Management
The use of medical cannabis in pain management represents a growing shift towards integrating more diverse therapeutic options in response to the complex nature of pain. With a historical context stretching back thousands of years, cannabis has re-emerged as a legitimate, albeit sometimes controversial, option for patients seeking relief from chronic pain.
Mechanism of Action

The effectiveness of medical cannabis in pain management is largely attributed to its interaction with the body’s endocannabinoid system (ECS), which plays a key role in regulating pain, mood, and homeostasis. Cannabinoids, like THC (tetrahydrocannabinol) and CBD (cannabidiol), bind to receptors in the ECS, namely CB1 and CB2 receptors. THC primarily interacts with CB1 receptors in the brain and nervous system, helping to alleviate pain and reduce inflammation. CBD works more indirectly by enhancing endocannabinoid signaling and modulating other receptors involved in pain perception.
Review of Research Studies and Clinical Trials
Numerous studies and clinical trials have evaluated the efficacy of cannabis in treating various types of pain, including neuropathic pain, fibromyalgia, and pain associated with multiple sclerosis and cancer. Results typically indicate that cannabis is effective in reducing pain intensity, improving sleep, and enhancing overall quality of life. For instance, cannabinoids have been found to reduce neuropathic pain significantly in patients unresponsive to standard pain therapy.
Legal and Medical Considerations
While the therapeutic potential of medical cannabis is promising, it also involves several legal and medical considerations:
- Legal status: The legal status of cannabis varies widely by region, affecting accessibility for patients and prescribing practices for healthcare providers.
- Medical guidelines: Due to the variability in cannabis strains and individual responses to cannabinoids, establishing standardized medical guidelines for dosing and administration poses challenges.
- Potential side effects and interactions: Like all treatments, cannabis use can carry risks, including psychological effects, potential dependency, and interactions with other medications.
Medical cannabis represents a complex but valuable addition to the pain management arsenal. For patients and healthcare providers, understanding the legal landscape, the biological mechanisms at play, and the empirical evidence supporting its use is crucial for making informed treatment decisions. As research progresses and legalization expands, medical cannabis is likely to play an increasingly prominent role in holistic pain management strategies.
Conclusion
In exploring the neurology of pain and the role of medical cannabis in pain management, we’ve delved into the complex interplay between the brain, body, and psychological factors that shape our experience of pain. Pain is not merely a physical sensation but a multifaceted phenomenon influenced by a myriad of neurological and emotional processes. The introduction of medical cannabis into the pain management spectrum represents a significant shift towards more personalized and holistic treatment approaches, acknowledging the diverse needs and responses of individuals suffering from chronic pain. As research continues to evolve and societal attitudes towards cannabis change, it is imperative for both patients and healthcare providers to stay informed about the latest developments and consider all available options to enhance quality of life for those affected by chronic pain. This comprehensive approach to understanding and managing pain, integrating both traditional and emerging therapies, promises not only relief but also a deeper understanding of the human condition.

Dr. Kashouty, a diplomate of the American Board of Psychiatry and Neurology (ABPN), practices general neurology with fellowship trained specialization in clinical neurophysiology. Dr. Kashouty finds the form and function of the nerves and muscles the most interesting part of neurology, which is what led him to specialize in neurophysiology with more emphasis on neuromuscular conditions. He treats all neurological diseases, but his main focus is to treat and manage headaches, movement disorders and neuromuscular diseases.




