In the intricate nexus of chronic pain management, especially within the realm of neurological conditions, patients and healthcare providers are continuously searching for effective and sustainable alternatives to conventional treatments. Amidst this quest, cannabis emerges as a compelling candidate, promising relief for those grappling with the relentless discomfort associated with neurological disorders such as multiple sclerosis, neuropathy, and Parkinson’s disease. Traditional pain management strategies often fall short in addressing the unique complexities of neurological pain, propelling interest towards the therapeutic potential of cannabis. This blog aims to delve deep into the role of cannabis in managing chronic pain tied to neurological conditions, exploring its mechanisms, the scientific evidence backing its use, patient experiences, and the legal landscape surrounding its application. By offering a comprehensive overview, we strive to illuminate the possibilities that cannabis presents for enhancing the quality of life for individuals afflicted by neurological conditions and their associated chronic pain.
In This Blog:
- Understanding Neurological Conditions and Associated Pain
- Overview of Cannabis and Its Components
- How to Use Cannabis for Neurological Pain
- FAQs About Cannabis for Neurological Pain
Understanding Neurological Conditions and Associated Pain
Neurological conditions encompass a wide range of disorders affecting the nervous system, each presenting unique challenges and symptoms for patients. Among these, chronic pain emerges as a prevalent and debilitating aspect, significantly impacting the quality of life for individuals affected by such conditions. Neuropathic pain, often described as shooting, burning, or electric shock-like sensations, is a common feature across many neurological disorders. Conditions such as diabetic neuropathy, post-herpetic neuralgia, and trigeminal neuralgia exemplify this type of pain, where damage or dysfunction in the nerves leads to abnormal signaling and chronic discomfort.
In addition to neuropathic pain, other neurological conditions such as multiple sclerosis (MS), Parkinson’s disease, and fibromyalgia are frequently accompanied by chronic pain. In MS, for example, individuals may experience a range of pain types, including musculoskeletal pain, neuropathic pain, and trigeminal neuralgia. This pain can arise from various mechanisms, including inflammation, demyelination, and central nervous system dysfunction. Similarly, Parkinson’s disease may cause muscle rigidity, tremors, and dystonia, leading to significant discomfort and pain for patients.
The complexity of neurological conditions extends beyond the physical symptoms, often impacting cognitive function, mood, and overall well-being. Chronic pain associated with these disorders not only affects individuals physically but also psychologically and socially, contributing to increased disability and decreased quality of life.
Understanding the multifaceted nature of neurological conditions and their associated pain is crucial for developing comprehensive treatment approaches that address the underlying pathology while effectively managing symptoms. In the following sections, we delve into the potential role of cannabis in alleviating chronic pain within the context of neurological disorders, exploring its mechanisms of action, therapeutic benefits, and practical considerations for patients and healthcare providers alike.
Overview of Cannabis and Its Components
Cannabis, also known as marijuana, has garnered increasing attention in recent years for its potential therapeutic benefits in managing chronic pain and various other medical conditions. At the heart of cannabis’s pharmacological properties are two primary components: tetrahydrocannabinol (THC) and cannabidiol (CBD).
Tetrahydrocannabinol (THC):
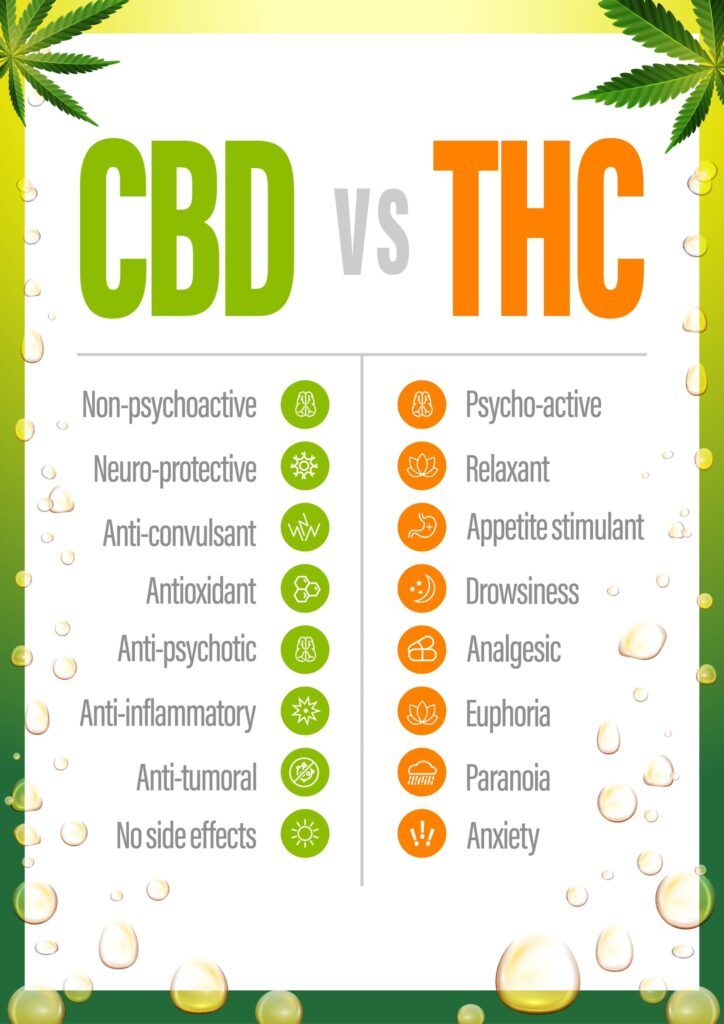
THC is the psychoactive compound in cannabis responsible for the euphoric “high” commonly associated with marijuana use. It interacts with cannabinoid receptors in the brain and central nervous system, particularly the CB1 receptors, to produce its psychoactive effects. Beyond its psychotropic properties, THC also exhibits analgesic, anti-inflammatory, and muscle-relaxant properties, making it a potentially valuable therapeutic agent for pain management.
Cannabidiol (CBD):
CBD is another prominent cannabinoid found in cannabis, although it lacks the psychoactive effects of THC. Instead, CBD interacts with various receptors in the body’s endocannabinoid system, including CB1 and CB2 receptors, as well as other non-cannabinoid receptors like serotonin receptors. CBD is known for its anti-inflammatory, analgesic, anxiolytic, and neuroprotective properties, making it a promising candidate for managing chronic pain and other medical conditions without the intoxicating effects associated with THC.
Mechanism of Action:
Both THC and CBD exert their effects by interacting with the body’s endocannabinoid system (ECS), a complex network of cannabinoid receptors and endocannabinoids found throughout the body. The ECS plays a crucial role in regulating various physiological processes, including pain perception, inflammation, mood, appetite, and sleep. THC and CBD mimic the actions of endocannabinoids, such as anandamide and 2-arachidonoylglycerol, by binding to cannabinoid receptors and modulating neurotransmitter release.
In addition to their interactions with the ECS, THC and CBD also exert their effects through other mechanisms, such as influencing the activity of neurotransmitters like dopamine, serotonin, and glutamate. These interactions contribute to cannabis’s diverse pharmacological effects, including pain relief, mood modulation, appetite stimulation, and anti-inflammatory actions.
By understanding the components of cannabis and how they work within the body, researchers and healthcare providers can better appreciate its potential therapeutic applications in managing chronic pain and other medical conditions. In the following sections, we explore the scientific evidence supporting the use of cannabis in alleviating chronic pain associated with neurological conditions, as well as practical considerations for its use in clinical practice.
How to Use Cannabis for Neurological Pain
Utilizing cannabis for managing neurological pain requires careful consideration of various factors, including the individual’s medical history, pain severity, tolerance, and preferences. Here, we explore the different methods of cannabis consumption and offer guidance on their potential effectiveness and considerations for use:
1. Inhalation:
- Smoking: Inhaling cannabis smoke provides rapid onset of effects, making it suitable for acute pain relief. However, smoking may irritate the lungs and respiratory system, posing risks for individuals with respiratory conditions.
- Vaporization: Vaporizing cannabis heats the plant material or concentrates to a temperature that releases cannabinoids and terpenes without combustion, reducing exposure to harmful toxins found in smoke. Vaporization offers similar rapid onset of effects as smoking but with potentially lower respiratory risks.
2. Oral Ingestion:

- Edibles: Cannabis-infused edibles, such as gummies, chocolates, and baked goods, offer a convenient and discreet method of consumption. However, onset of effects may be delayed (typically 30 minutes to 2 hours) due to digestion, making it challenging to titrate dosage. Caution is advised to prevent accidental overconsumption, which can lead to adverse effects.
- Tinctures and Oils: Sublingual administration of cannabis tinctures or oils involves placing drops under the tongue for rapid absorption into the bloodstream. This method allows for precise dosing and easier titration compared to edibles.
3. Topical Application:
- Topical Creams and Balms: Cannabis-infused creams, lotions, and balms can be applied directly to the skin over the affected area for localized pain relief. While topical application bypasses the psychoactive effects associated with systemic absorption, it may offer limited efficacy for neuropathic pain that originates deep within the body.
Dosage Considerations:
- Start Low, Go Slow: Begin with a low dose of THC and/or CBD and gradually increase as needed to achieve desired pain relief while minimizing potential side effects.
- Individualized Approach: Cannabis affects each person differently, so it’s essential to tailor dosage and consumption methods based on individual responses and tolerance levels.
- Consultation with Healthcare Providers: Seek guidance from healthcare professionals experienced in cannabis therapeutics to develop personalized treatment plans and monitor for potential interactions with existing medications.
Legal and Regulatory Considerations:
- Adherence to Local Laws: Familiarize oneself with the legal status of medical cannabis in one’s jurisdiction and obtain necessary prescriptions or recommendations from healthcare providers.
- Quality Assurance: Choose cannabis products from reputable sources that undergo rigorous testing for potency, purity, and safety.
By understanding the various methods of cannabis consumption and dosage considerations, individuals can make informed decisions about incorporating cannabis into their pain management regimen. However, it is crucial to approach cannabis use for neurological pain with caution and seek guidance from healthcare professionals to ensure safe and effective treatment outcomes.
FAQs About Cannabis for Neurological Pain
1. Is cannabis legal for treating neurological pain?
The legal status of cannabis for medical use varies widely depending on jurisdiction. While some regions have legalized medical cannabis, others maintain strict regulations or prohibit its use entirely. It’s essential to familiarize yourself with the laws and regulations in your area regarding medical cannabis use and consult with healthcare professionals for guidance on obtaining legal access. In Florida, patients seeking medical cannabis must have one of the listed Debilitating Medical Conditions.
2. How does cannabis alleviate neurological pain?
Cannabis contains compounds called cannabinoids, such as THC and CBD, which interact with the body’s endocannabinoid system to modulate pain perception, inflammation, and other physiological processes. THC has analgesic and anti-inflammatory properties, while CBD exhibits analgesic, anti-inflammatory, and neuroprotective effects. Together, these cannabinoids may help alleviate neurological pain by targeting various pathways involved in pain transmission and modulation.
3. What are the potential side effects of using cannabis for neurological pain?

Common side effects of cannabis use include dizziness, drowsiness, dry mouth, and impaired coordination. In some cases, particularly with high THC concentrations, individuals may experience anxiety, paranoia, or cognitive impairment. Long-term cannabis use may also pose risks for dependency and addiction. It’s crucial to start with low doses, monitor for adverse effects, and consult healthcare professionals for personalized guidance on managing side effects.
4. Can cannabis interact with other medications for neurological conditions?
Yes, cannabis may interact with other medications commonly prescribed for neurological conditions, such as anticonvulsants, antidepressants, and muscle relaxants. THC and CBD can affect the metabolism of certain medications by inhibiting or inducing enzymes in the liver responsible for drug metabolism, potentially altering their efficacy or increasing the risk of adverse effects. It’s essential to disclose all medications and supplements to healthcare providers and seek their advice on potential drug interactions before using cannabis.
5. What is the scientific evidence supporting the use of cannabis for neurological pain?
While anecdotal reports and some clinical studies suggest that cannabis may offer relief for neurological pain, the scientific evidence remains limited and inconclusive. More research, including well-designed clinical trials, is needed to establish the safety, efficacy, and optimal dosing of cannabis for treating neurological pain. However, preliminary findings indicate that cannabis, particularly formulations containing balanced ratios of THC and CBD, may hold promise as an adjunctive therapy for managing neurological pain in certain individuals.
Conclusion
As we navigate the evolving landscape of pain management, particularly for those enduring the complexities of chronic pain associated with neurological conditions, cannabis stands out as a beacon of hope, offering a potential path to relief where traditional methods may falter. The anecdotes, studies, and scientific evidence discussed underscore the necessity for a personalized, informed approach to incorporating cannabis into pain management regimens. However, the journey doesn’t end here. Ongoing dialogue, research, and education are paramount to unlocking the full potential of cannabis in alleviating neurological pain. We encourage readers to engage in this conversation—share your experiences, ask questions, and seek advice from healthcare professionals. Together, through sharing knowledge and advocating for further research, we can pave the way for more effective, compassionate treatment options for those struggling with the profound impact of chronic pain. Let’s not just envision a future of improved pain management; let’s actively participate in shaping it.

Dr. Kashouty, a diplomate of the American Board of Psychiatry and Neurology (ABPN), practices general neurology with fellowship trained specialization in clinical neurophysiology. Dr. Kashouty finds the form and function of the nerves and muscles the most interesting part of neurology, which is what led him to specialize in neurophysiology with more emphasis on neuromuscular conditions. He treats all neurological diseases, but his main focus is to treat and manage headaches, movement disorders and neuromuscular diseases.




