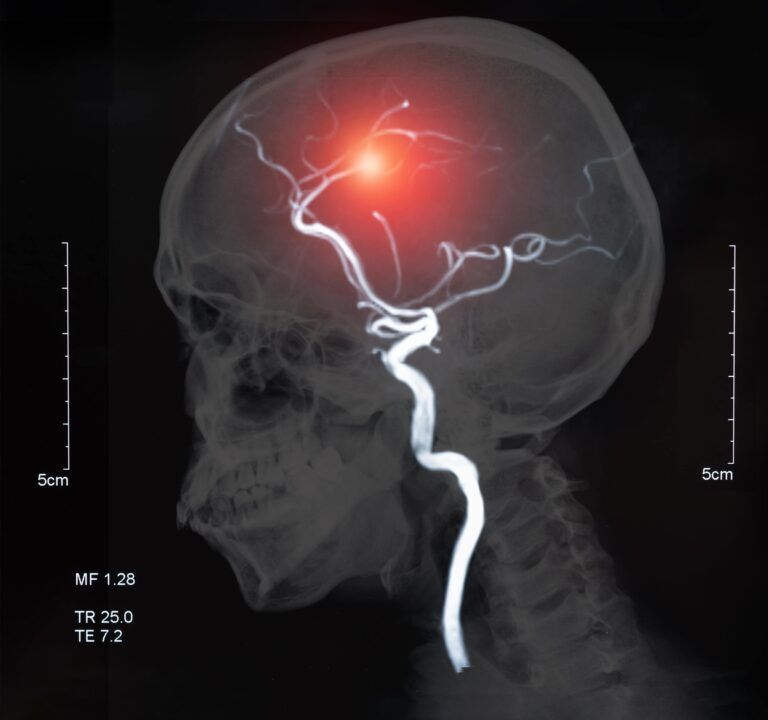
Strokes are a major health concern worldwide, known for their sudden and often devastating impact on health. They occur when the blood supply to part of the brain is interrupted or reduced, preventing brain tissue from getting oxygen and nutrients. This blog aims to shed light on the different types of strokes, their causes, symptoms, and treatment, emphasizing the importance of early detection and prevention.
Ischemic Strokes
Ischemic strokes are the most common type of stroke, accounting for approximately 87% of all stroke cases. They occur when the arteries to the brain become narrowed or blocked, causing a significant reduction in blood flow (ischemia). The reduction or interruption in blood flow deprives the brain tissue of oxygen and nutrients, which can lead to the death of brain cells within minutes.
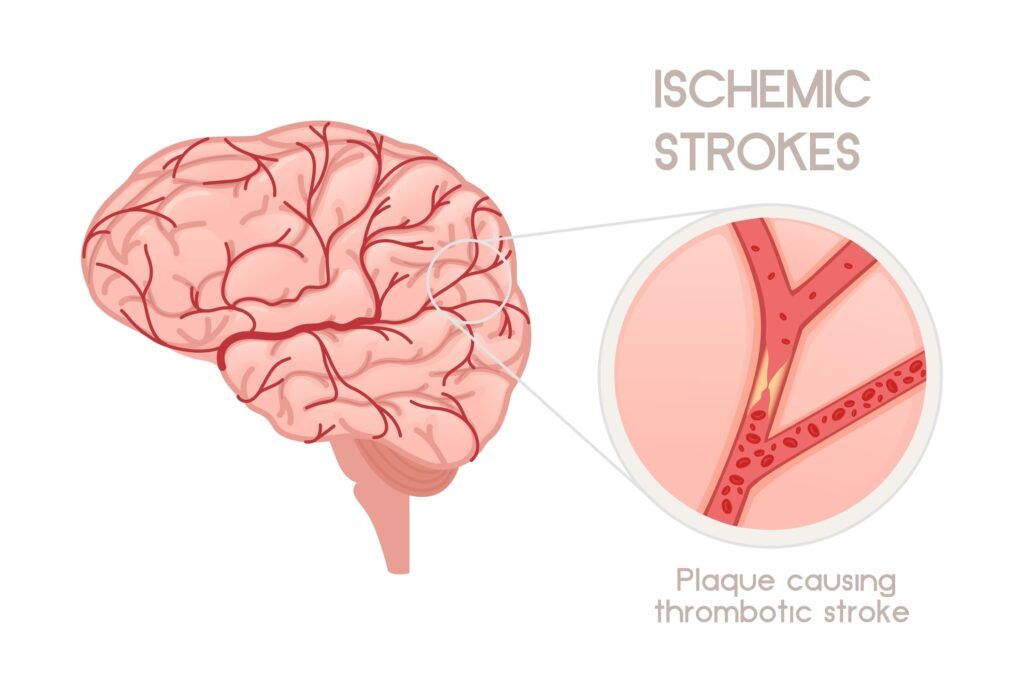
Causes of Ischemic Strokes:
- Thrombotic Stroke: This happens when a blood clot (thrombus) forms in one of the arteries that supply blood to the brain. This type of stroke is often seen in people with high cholesterol levels and atherosclerosis.
- Embolic Stroke: This type of ischemic stroke occurs when a blood clot or other debris forms away from the brain — commonly in the heart — and is swept through the bloodstream to lodge in narrower brain arteries. This type of clot is called an embolus.
Risk Factors:
- Hypertension (high blood pressure)
- High cholesterol
- Diabetes
- Smoking
- Obesity
- Cardiovascular diseases, such as heart failure, atrial fibrillation, and heart defects.
Symptoms:
- Sudden numbness or weakness in the face, arm, or leg, especially on one side of the body
- Trouble speaking or understanding speech
- Vision problems in one or both eyes
- Difficulty walking, dizziness, loss of balance or coordination
- Sudden, severe headache with no known cause
Hemorrhagic Strokes
Hemorrhagic strokes occur when a blood vessel in the brain leaks or ruptures. This type of stroke is less common than ischemic strokes, accounting for about 13% of stroke cases, but is often more deadly. The bleeding from a hemorrhagic stroke can damage brain cells, and the accumulation of blood can increase pressure within the skull, causing further harm.
Hemorrhagic strokes can be classified into two main types:
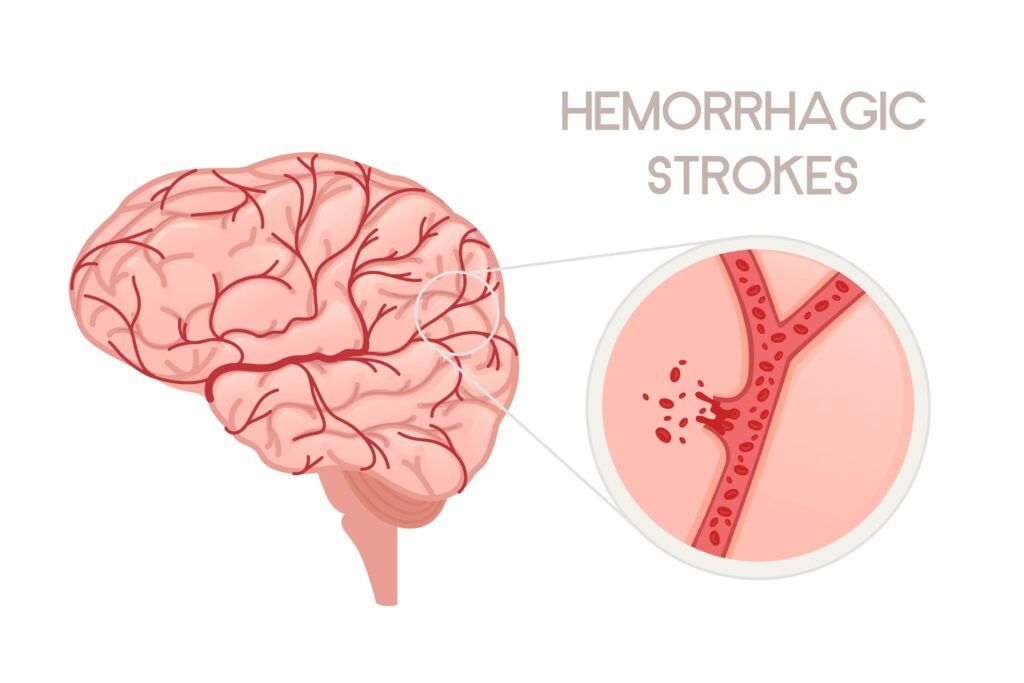
- Intracerebral Hemorrhage (ICH):
- This is the most common type of hemorrhagic stroke, occurring when a blood vessel inside the brain bursts and leaks blood into surrounding brain tissue.
- Causes include high blood pressure (hypertension), overuse of anticoagulant medication, aneurysms, or head trauma.
- Symptoms may include sudden, severe headache, weakness, numbness, or paralysis, especially on one side of the body, difficulty speaking or swallowing, vision problems, loss of balance or coordination, and altered consciousness or confusion.
- Subarachnoid Hemorrhage (SAH):
- This type of hemorrhagic stroke involves bleeding into the subarachnoid space, the area between the brain and the thin tissues that cover it.
- The most common cause is the rupture of an aneurysm, a weak spot in a blood vessel wall. Other causes include arteriovenous malformations (AVMs), head injury, and blood disorders.
- Symptoms often include a sudden and severe headache, often described as the “worst headache of my life,” along with neck pain, nausea, vomiting, light sensitivity, and seizures.
Risk Factors for Hemorrhagic Strokes:
- Chronic high blood pressure is the most significant risk factor
- Smoking
- Excessive alcohol use
- Use of blood-thinning medications
- Family history of hemorrhagic strokes
Symptoms of Hemorrhagic Strokes:
The symptoms are similar to those of ischemic strokes but can also include more severe headaches, nausea, vomiting, and decreased levels of consciousness.
Transient Ischemic Attacks (TIAs)
Transient Ischemic Attacks (TIAs), often referred to as “mini-strokes,” are brief episodes of stroke-like symptoms that occur due to a temporary decrease in blood supply to part of the brain. Unlike strokes, the symptoms of a TIA are temporary and usually resolve within a few minutes to 24 hours, typically without causing permanent brain damage.
Causes:
- Similar to ischemic strokes, TIAs are often caused by a temporary clot or blockage in an artery leading to the brain.
- The blockage could be due to blood clots, arterial plaque, or other blood or artery conditions.
Symptoms:
The symptoms of a TIA mimic those of a stroke and can include:
- Sudden numbness or weakness, particularly on one side of the body
- Confusion
- Trouble speaking or understanding speech
- Vision problems in one or both eyes
- Dizziness, loss of balance, or coordination.
Unlike a stroke, these symptoms are temporary and usually resolve quickly.
Significance:
- TIAs are important warning signs of a possible future stroke. Approximately 1 in 3 people who experience a TIA go on to have a subsequent stroke, often within a year.
- Prompt medical evaluation after a TIA is crucial to determine the cause and to implement preventive strategies to reduce the risk of a future stroke.
Stroke Prevention: Key Strategies to Reduce Your Risk
Stroke prevention is critically important as strokes can lead to significant disability and even death. However, the good news is that up to 80% of strokes may be preventable through lifestyle changes and medical interventions. Here are some key strategies to reduce the risk of stroke:
Lifestyle Modifications
Healthy Diet:
- Eating a diet rich in fruits, vegetables, whole grains, and lean proteins can help reduce stroke risk.
- Limiting intake of saturated fats, trans fats, and cholesterol can also lower the risk of artery blockage.
Regular Physical Activity:
- Engaging in moderate-intensity aerobic activity for at least 150 minutes per week can improve overall cardiovascular health.
- Activities like brisk walking, swimming, or cycling are beneficial.
Maintain a Healthy Weight:
- Overweight and obesity increase the risk of high blood pressure, diabetes, and atherosclerosis, all of which are stroke risk factors.
- A balanced diet and regular exercise can help maintain a healthy weight.
Quit Smoking:
- Smoking accelerates clot formation, thickens blood, and increases the amount of plaque buildup in the arteries.
- Quitting smoking can significantly reduce the risk of stroke.
Limit Alcohol Intake:
- Excessive alcohol consumption can lead to high blood pressure and increase the risk of stroke.
- It’s advised to limit alcohol to no more than two drinks per day for men and one drink per day for women.
Medical Management
Control Blood Pressure:

- High blood pressure is one of the leading causes of stroke. Managing blood pressure through diet, exercise, and medication is crucial.
- Regular monitoring and working with a healthcare provider to maintain a blood pressure below 130/80 mm Hg is recommended.
Manage Heart Disease:
- Conditions like atrial fibrillation, heart valve disease, and others can increase stroke risk.
- Appropriate treatment, which may include medications like blood thinners, can help manage these conditions.
Lower Cholesterol:
- High levels of LDL (bad) cholesterol can lead to plaque buildup in arteries, increasing stroke risk.
- Diet, exercise, and cholesterol-lowering medications like statins are effective in managing cholesterol levels.
Control Diabetes:
- Diabetes increases the risk of stroke by affecting blood vessels and promoting atherosclerosis.
- Managing blood sugar levels through diet, exercise, and medication can reduce stroke risk.
Regular Medical Checkups:
- Regular checkups can help detect and manage risk factors for stroke early.
- Blood pressure, cholesterol, and diabetes screenings are essential parts of these checkups.
Stroke Management
Stroke management is a critical and multifaceted process that begins with immediate medical intervention and continues through long-term rehabilitation. In the acute phase, rapid assessment and treatment are crucial to minimize brain damage and improve outcomes. For ischemic strokes, this often involves administering clot-busting drugs like tissue plasminogen activator (tPA) or performing mechanical thrombectomy to remove clots. In the case of hemorrhagic strokes, controlling bleeding and reducing intracranial pressure are priorities, sometimes requiring surgical interventions. Once the immediate crisis is managed, the focus shifts to rehabilitation, which is tailored to the individual’s specific needs and may involve a team of specialists including physical therapists, occupational therapists, speech therapists, and neuropsychologists. Rehabilitation aims to help the survivor regain as much function as possible and adapt to any remaining disabilities. Additionally, secondary prevention strategies, including lifestyle modifications and medications to manage risk factors like hypertension, diabetes, and high cholesterol, are vital to prevent recurrent strokes. Stroke management is a comprehensive approach that requires coordinated care and patient and family education to ensure the best possible recovery and quality of life post-stroke.
Conclusion
Understanding the different types of strokes, their symptoms, and risk factors is essential for prevention and early intervention. If you or someone you know is at risk or experiences symptoms of a stroke, immediate medical consultation is crucial. With ongoing research and advancements, there is hope for better treatments and recovery outcomes for stroke patients.

Dr. Kashouty, a diplomate of the American Board of Psychiatry and Neurology (ABPN), practices general neurology with fellowship trained specialization in clinical neurophysiology. Dr. Kashouty finds the form and function of the nerves and muscles the most interesting part of neurology, which is what led him to specialize in neurophysiology with more emphasis on neuromuscular conditions. He treats all neurological diseases, but his main focus is to treat and manage headaches, movement disorders and neuromuscular diseases.