Lumbrosacral Radiculopathy
Get Relief From Lower Back Pain
Premier Neurology & Wellness Center helps patients with conditions such as Lumbosacral Radiculopathy from our offices in Stuart, FL. Find relief with us.
Radiculopathy is injury of spinal nerves causing pain or numbness in arms and legs.
What is Radiculopathy?
Radiculopathy refers to disease or injury of the spinal nerve roots resulting in radicular pain, weakness, numbness and/or tingling in the arms or legs. Pain may be felt in a region corresponding to a dermatome, an area of skin innervated by the sensory fibers of a given spinal nerve. There are cervical (neck), thoracic (middle back), and lumbosacral (lower back) radiculopathies depending on the location of the injury.
Radiculopathies are further categorized by what level of vertebrae they are associated with, therefore if the injury is at the neck region, the term cervical radiculopathy is used, if the injury is at the lower back, the term lumbosacral radiculopathy is used and so on.
FUNCTIONAL ANATOMY
Common Causes of Radiculopathy
Anatomy
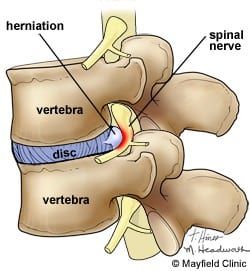
In the lower spine, there are five vertebrae and five lumbar nerve roots exist from the lumbar spine. Intervertebral discs are located between the vertebral bodies of L1-L5. The discs are composed of outer and inner fibrotic tissues and serve as a protective barrier between the vertebrae.
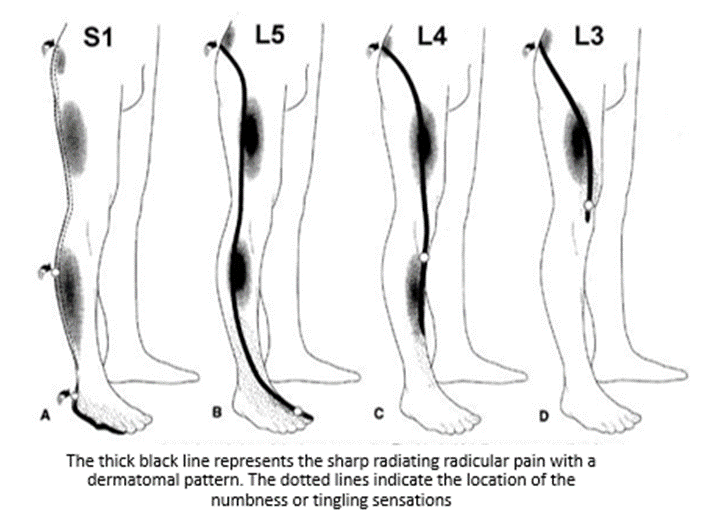
Radiculopathies are categorized according to which part of the spinal cord is affected. For example, if the nerve root between the third and fourth vertebrae is injured, the L3 or L4 nerve root will be pinched or strained therefore the term L3 or L4 radiculopathy will be used and so on.
Where and How
The two most common nerve roots that are affected in the lumbosacral region are the fifth lumbar (L5) and the first sacral (S1) roots. Each has a specific distribution of the pain, numbness and weakness patterns. An L5 radiculopathy causes pain that radiates from the buttock down the leg to the outside of the ankle and into the top of the foot toward the big toe. People experience numbness on the outside of the ankle and top of the foot. If severe, weakness in the leg muscles will result in a footdrop. This can often be detected by a slapping of the foot that occurs with each step. People often trip over small objects because they are unable to lift their foot when they walk. An S1 radiculopathy causes pain that runs from the buttock and the thigh into the calf and outside of the foot. The numbness is usually experienced on the outside of the foot. The weakness, when present involves the hamstring muscle which flexes the knee and the calf muscles which pushes the foot down.
Who gets affected?
Most people will experience some form of radiculopathy at some point in their lives. The radiculopathy occurs more often in the middle-aged and elderly than in the young, with the highest risk being for adults 40 to 60 years old. However, injuries due to sports, heavy lifting, or bad posture affect the young as well.
Radiculopathy can be caused by any disease or injury process that compresses or otherwise injures the spinal nerve root from trauma or falls, cancer, infections, diseases that lead to degeneration of the vertebrae and/or intervertebral discs (osteoarthritis), slipped or herniated discs, spine deformities (scoliosis), and other factors as well. Other less common causes are synovial cysts that arise from the facet joints and if they protrude into the spinal canal can compress a nerve root. Infections and tumors are also possible but are rare causes of nerve root compression. Spinal stenosis can result in severe leg pain and muscle stiffness but more often causes pain that is produced by activity such as walking.

Middle-Aged and Elderly patients are at highest risk of radiculpathy.
Diagnosis of Lumbosacral Radiculopathy
EMG
Patients with signs and symptoms that correlate to radiculopathy must have an electrodiagnostic study (Nerve conduction study and EMG) to confirm the diagnosis by a highly specialized and fellowship-trained neurologist such as Dr Yono and Dr Kashouty. Electrodiagnostic studies can help distinguish radiculopathy from other etiologies and is important in identifying physiologic abnormalities of the nerve roots and the muscles.
X-Rays Or MRI's
MRI has become the method of choice for imaging the lower back to detect significant soft-tissue pathology, such as disc bulge or herniation. The American College of Radiology recommends routine MRI as the most appropriate imaging study in patients with chronic low back pain who have neurologic signs or symptoms. MRI can detect ligament and disc disruption, which cannot be demonstrated by other imaging studies. The entire spinal cord, nerve roots, and axial skeleton can also be visualized in details.
All imaging studies must be used in conjunction with the patient’s history and physical
examination findings to make the diagnosis of radiculopathy.
Treatment
Treatment for radiculopathy varies with the nature and severity of the disease process or injury that has caused the disorder. Initial treatment must be directed at reducing pain and inflammation around the injured spinal nerve. The treatment can begin with local icing, medications to treat the pain such as nonsteroidal anti-inflammatory drugs NSAIDs (Ibuprofen, etc.), and measures that reduce the pressure on the nerve root. This consists of relative rest, avoiding positions that add extra strain on the lower back. Patient-specific exercises are prescribed by a physical therapist for the targeted strengthening of the lower back muscles and other supporting tissues to relieve pressure on affected spinal nerve roots.
Epidural corticosteroid injections, selective nerve root block, and epidural lysis (destruction) of adhesions are considered as secondary treatment options to treat radiculopathy. Epidural steroid injections have been used in patients whose conditions have not had satisfactory responses to medications, and a well-designed physical therapy program. Acupuncture has also been used to treat radicular pain in conjunction with other treatments with some success.
When conservative treatment fails, spinal surgery may be needed. The primary purpose of surgery is to stop the progression of symptoms by relieving the pressure on the affected spinal nerve roots. Procedures may include laminectomy, discectomy and fusion which will be discussed in detail with the spinal surgeon. With appropriate indications, surgery can result in resolution of symptoms and excellent outcomes in the majority of patients.